use plamasphresis for triglyceride induced pancreatitis
- related: GI gastroenterology
- tags: #GI #icu #literature

Lipemic blood sample from the patient.
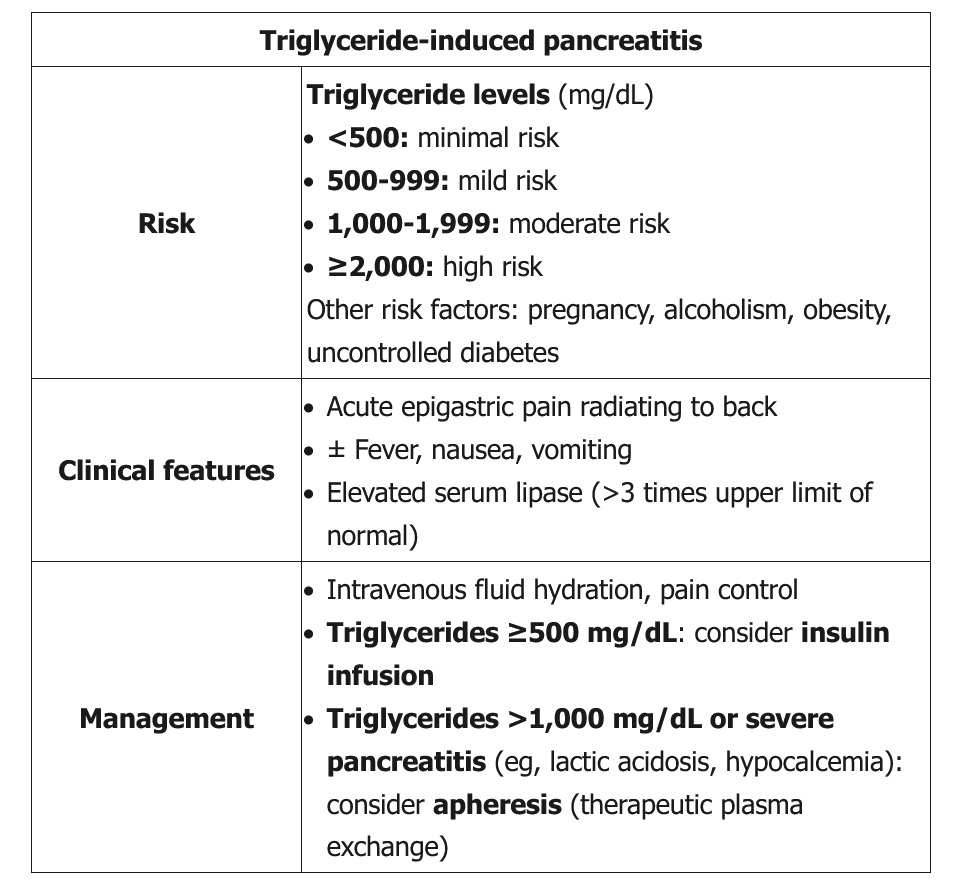
This patient has acute pancreatitis, likely due to hypertriglyceridemia. Pancreatitis can occur in primary (inherited) or acquired hypertriglyceridemia, and the risk increases with pregnancy, alcohol intake, obesity, and uncontrolled diabetes. The risk also increases across all levels of hypertriglyceridemia, but most cases occur in patients with visibly lipemic serum and triglyceride levels **>1,000 mg/dL**.
Initial management is similar to that for pancreatitis from other causes and includes supportive care (eg, intravenous hydration, pain control). In addition, moderate to severe hypertriglyceridemia-induced pancreatitis (eg, triglycerides >1,000 mg/dL, lipase ≥>3 times the upper limit of normal, evidence of organ dysfunction) requires rapid lowering of serum triglyceride levels:
- If triglyceride levels are >1,000 mg/dL or pancreatitis is severe (eg, lactic acidosis, acute kidney injury, hypocalcemia), as in this patient, therapeutic plasma exchange (apheresis) should be considered to quickly lower triglyceride levels.
- If triglyceride levels are ≥500 mg/dL, an insulin infusion (with intravenous glucose to prevent hypoglycemia when glucose falls below 200 mg/dL) can correct triglyceride levels within 3-4 days by enhancing lipoprotein lipase activity.
Insulin lowers triglyceride levels by activating lipoprotein lipase and can result in significant reduction of serum triglyceride levels over 1 to 3 days. It is a first-line therapy in the management of patients with HTG-AP who have concomitant hyperglycemia and can be considered in patients without hyperglycemia who have severe HTG-AP (choice A is correct). Regular insulin is generally administered as a continuous infusion at 0.1 to 0.3 units/kg/h. Patients should be monitored for hypoglycemia and receive dextrose and/or nutrition while receiving continuous insulin. Insulin can be discontinued when serum triglyceride levels fall below 500 mg/dL (5.6 mmol/L)
Insulin infusion can also be used if plasma exchange is unavailable or not tolerated.
Ultrafiltration and hemodialysis do not remove larger molecules and lipoproteins and therefore are not useful in this patient.
Mild triglyceride-induced pancreatitis (ie, triglycerides <1,000 mg/dL, lipase ≤3 times the upper limit of normal, normal calcium level, no evidence of end-organ damage) can sometimes be managed conservatively, and triglyceride levels fall gradually while the patient is fasting. However, this patient has clinical features (eg, hypocalcemia, acute kidney injury) that warrant more aggressive management.
Once the patient’s condition has been stabilized, long-term management should include dietary fat restriction and triglyceride-lowering medication (eg, gemfibrozil). However, these medications would not lower lipids rapidly enough to avoid further pancreatic injury.
HTG is the third most common cause of acute pancreatitis in the general population and the second most common cause of acute pancreatitis in pregnancy. The pathophysiological mechanisms that drive acute pancreatitis in patients with severe HTG are not fully understood. There are numerous hypotheses, but it is proposed that hydrolysis of excess TGs by pancreatic lipase results in increased formation of free fatty acids (FFAs), which are toxic to acinar cells, causing inflammation in the pancreas, and FFA-mediated endothelial dysfunction may lead to acute lung injury and multiorgan failure in HTG-induced acute pancreatitis. Pancreatitis is typically seen when TG levels are greater than 500 mg/dL (5.65 mmol/L). Conservative treatment with fasting, fluid resuscitation, and analgesia is the treatment of choice for the majority of patients with HTG-induced acute pancreatitis. However, a subset of patients with severe pancreatitis and associated organ dysfunction may benefit from additional interventions to decrease TG levels more rapidly.
Plasmapheresis has been used in the treatment of HTG-induced acute pancreatitis since the 1970s. Evidence from randomized and nonrandomized studies have shown a more rapid reduction of TG levels in the first 24 h with plasmapheresis compared with results with conservative therapy plus insulin infusion. However, plasmapheresis comes with additional costs and potential complications, and the evidence is less clear on whether rapid TG lowering is associated with improved, patient-centered clinical outcomes. Thus, routine use of plasmapheresis is not indicated in nonsevere HTG-induced acute pancreatitis. The generally accepted role for plasmapheresis is for patients such as the patient in this case, with extremely high TG levels (> ~4,400 mg/dL [>49.72 mmol/L]); in patients with severe HTG-induced acute pancreatitis as evidenced by hypocalcemia, elevated lactate levels, signs of severe systemic inflammation, and/or signs of multiorgan dysfunction or failure; or in patients who do not improve despite other therapies, including insulin infusion. Because treatment strategies are mostly expert opinion based on limited data from small studies, personal experience, and mechanistic pathways, treatment strategies vary across medical centers, informed by center experience, availability of apheresis, and local expert opinions. Among the provided answer choices, only plasmapheresis would be expected to lower this patient’s TG level rapidly.
Unfractionated heparin infusions were used in the past in the treatment of HTG-induced acute pancreatitis because heparin targets TG and FFA metabolism. Heparin releases endothelial lipase and transiently increases circulating lipoprotein lipase (LPL) levels. LPL hydrolyzes circulating TGs into FFAs, initially decreasing TG levels, but later causes LPL deficiency owing to increased hepatic metabolism. For this reason, and because of the theoretical increased risk of bleeding into a necrotic pancreas, heparin is no longer recommended in HTG-induced acute pancreatitis.
Gemfibrozil is sometimes recommended as long-term therapy as a patient is recovering from HTG-induced acute pancreatitis in order to prevent recurrent episodes of pancreatitis and other consequences of HTG. However, this medication is not used in the acute phase of HTG-induced acute pancreatitis. Continuous renal replacement therapy is not used as a management strategy for patients with HTG-induced acute pancreatitis, outside of the typical indications for renal replacement therapy, which are not present in this case.1234
Links to this note
Footnotes
-
Dhindsa S, Sharma A, Al-Khazaali A, et al. Intravenous insulin versus conservative management in hypertriglyceridemia-associated acute pancreatitis. J Endocr Soc. 2020;4(1):bvz019. PubMed ↩
-
Gubensek J. The role of apheresis and insulin therapy in hypertriglyceridemic acute pancreatitis-a concise review. BMC Gastroenterol. 2023;23(1):341. PubMed ↩
-
Newman CB, Blaha MJ, Boord JB, et al. Lipid management in patients with endocrine disorders: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2020;105(12):dgaa674. PubMed ↩