use pulmonary artery catheter in heart failure patients
- related: Cardiology
- tags: #literature #cardiology
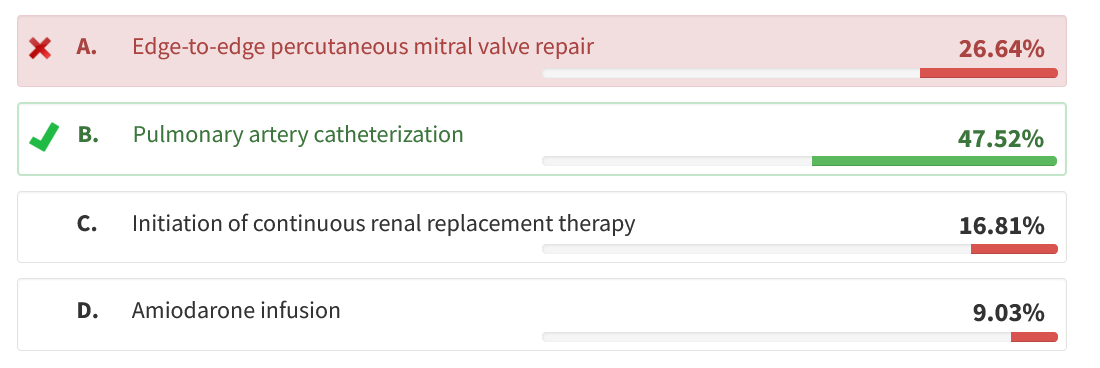
This patient has advanced heart failure and is failing to respond to empiric therapy with continuous diuretic infusion and milrinone. She has persistent hypotension and worsening renal function. Given that the patient has been refractory to initial challenge with inotropes and IV diuretics, the best next step would be to pursue pulmonary artery catheterization to characterize intravascular hemodynamics and to guide therapy. This is also a necessary first step in an evaluation for advanced therapies, including durable left ventricular assist devices and cardiac transplantation (choice B is correct).
The randomized ESCAPE trial is often cited as providing evidence that pulmonary artery catheterization does not change outcomes in patients with heart failure, but that trial excluded patients with recent inotropic therapy and so would not apply in cases such as this. In fact, several prospective series have reported improved outcomes when pulmonary artery catheters are used in patients with cardiogenic shock. Failure to respond to empiric inotropic therapy and uncertainty about intravascular volume status are very good reasons to consider invasive hemodynamic assessment, as it might allow titration of diuretics and vasoactive agents to maximize cardiac output while minimizing arrhythmias and myocardial oxygen consumption. Measurement of mixed venous oxygen saturation, which can be done only with a catheter in the pulmonary artery, can also inform the adequacy of cardiac output.
Percutaneous mitral valve repair has been shown to reduce morbidity and mortality in patients with severe mitral regurgitation disproportionate to the degree of left ventricular dilation who are symptomatic despite optimal medical therapy but has not been shown to improve outcomes in patients with cardiogenic shock on inotropic therapy (choice A is incorrect).
Continuous renal replacement therapy can be useful in achieving a negative volume balance in patients with cardiogenic shock, low BP, and volume overload, but this patient continues to respond to IV diuretics and does not meet any other criteria to initiate renal replacement therapy (choice C is incorrect).
While this patient has had several episodes of asymptomatic nonsustained ventricular tachycardia, this was likely an adverse effect of milrinone infusion, and antiarrhythmic drugs are not indicated (choice D is incorrect).12345
A 62-year old woman with nonischemic cardiomyopathy and chronic heart failure with reduced ejection fraction is admitted with acute decompensated heart failure. Medical history includes hypertension, diabetes, and chronic kidney disease with a baseline creatinine of 1.6 mg/dL (141.44 µmol/L). Her regimen consists of torsemide, carvedilol, spironolactone, sacubitril-valsartan, and dapagliflozin along with metformin. She has had two heart failure hospitalizations over the past 6 months.
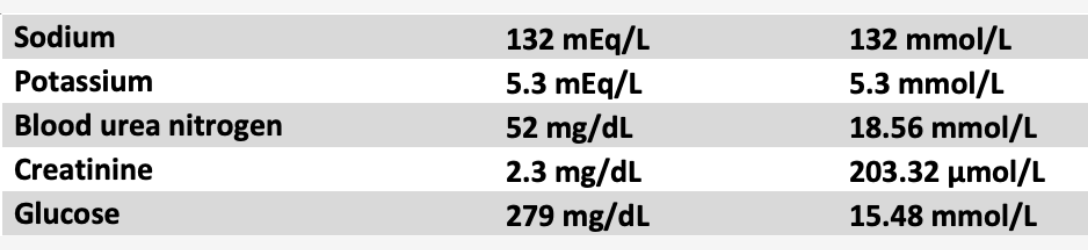
On presentation, BP is 92/68 mm Hg and heart rate is 112/min. Jugular venous pressure is 12 mm Hg, she has bibasilar crackles, holosystolic murmur at the apex, S3 gallop, and 2+ bilateral edema. Laboratory values at presentation are shown in Figure 1.
She is admitted to the cardiac ICU. Echocardiography shows a dilated left ventricle with end-systolic dimension 7.4 cm, severe global hypokinesis, and estimated ejection fraction of 20%. Additional findings include severe central mitral regurgitation, moderate tricuspid regurgitation, and estimated right ventricular systolic pressure of 55 mm Hg. The neurohormonal agents are stopped, and she is started on continuous infusions of furosemide at 20 mg/h and milrinone at 0.125 µg/kg/min. Urine output is 2.4 L over the first 24 h, but when milrinone is increased to 0.25 µg/kg/min, she has several episodes of asymptomatic, nonsustained ventricular tachycardia. Repeat laboratory tests show a sodium level of 130 mEq/L (130 mmol/L), potassium level of 5.2 mEq/L (5.2 mmol/L), blood urea nitrogen level of 64 mg/dL (22.85 mmol/L), and creatinine level of 2.7 mg/dL (238.68 µmol/L).
Which of the following is the most appropriate next step in her management?
Links to this note
Footnotes
-
Binanay C, Califf RM, Hasselblad V, et al; ESCAPE Investigators and ESCAPE Study Coordinators. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625-1633. PubMed ↩
-
Fang JC, Ewald GA, Allen LA, et al; Heart Failure Society of America Guidelines Committee. Advanced (stage D) heart failure: a statement from the Heart Failure Society of America Guidelines Committee. J Card Fail. 2015;21(6):519-534. PubMed ↩
-
Hollenberg SM, Warner Stevenson L, Ahmad T, et al. 2019 ACC expert consensus decision pathway on risk assessment, management, and clinical trajectory of patients hospitalized with heart failure: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2019;74(15):1966-2011. PubMed ↩
-
Writing Committee, Maddox TM, Januzzi JL Jr, et al. 2021 Update to the 2017 ACC expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2021;77(6):772-810. PubMed ↩