use stress echo in aortic stenosis
- related: Cardiology
- tags: #literature #cardiology
This patient presented with congestive heart failure in the setting of aortic stenosis and severe left ventricular dysfunction. The key issue is the severity of the aortic stenosis and whether this is the cause of the pulmonary edema. She has a low cardiac output (stroke volume of 30 mL at a heart rate of 90/min yields an output of 2.7 L/min); thus, although the gradient across her aortic valve is low, she meets criteria for low output aortic stenosis (cardiac index <3.0 L/min/m2, mean gradient <30 mm Hg). The challenge is to distinguish pseudostenosis, in which low cardiac output reduces valve opening forces, so the severity of moderate aortic stenosis is overestimated, from severe aortic stenosis with secondary left ventricular dysfunction that leads to a low transvalvular gradient. The distinction is important because patients with pseudostenosis are unlikely to benefit from either surgical or transcatheter valve replacement. Dobutamine can be used to make the distinction between true aortic stenosis and pseudostenosis. If dobutamine increases cardiac output and the valve gradient is unchanged, then calculated valve area will increase, indicating pseudostenosis. If cardiac output increases and the valve gradient increases to a commensurate degree, then true aortic stenosis is confirmed. If cardiac output fails to increase (that is, the patient lacks contractile reserve), then the test is indeterminate with regard to the severity of the aortic stenosis but still retains some value, since patients without contractile reserve have a poor prognosis with or without valve replacement
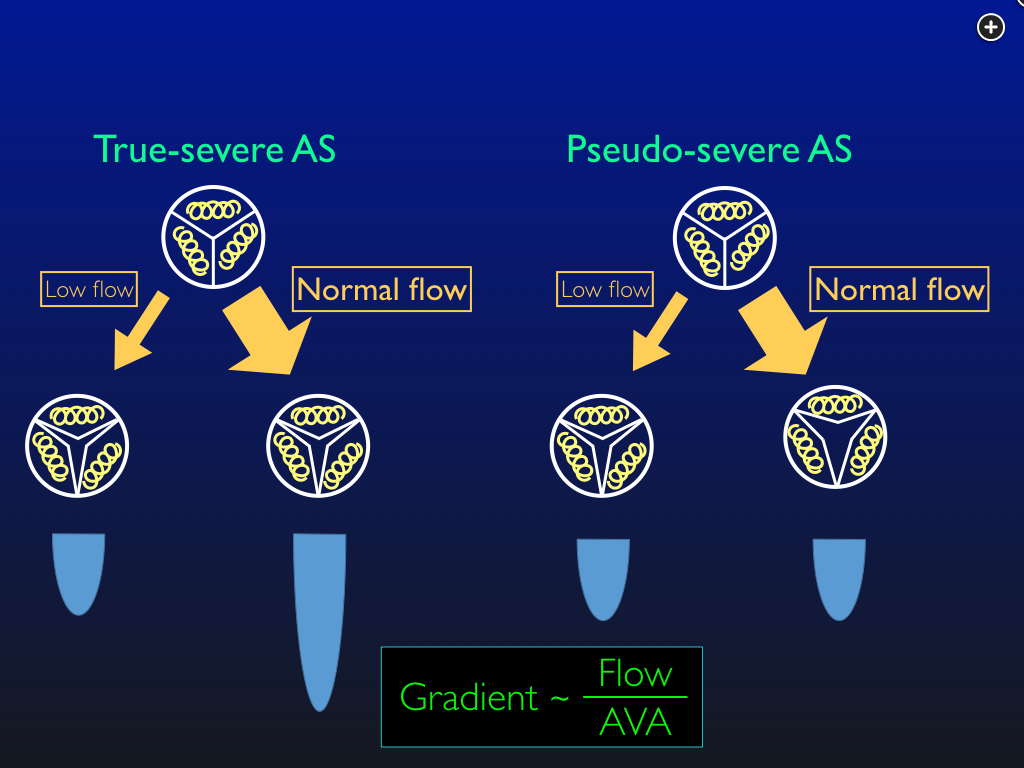
Dobutamine stress echocardiography to distinguish true severe aortic stenosis from pseudo-severe AS. With true AS, an increase in flow with dobutamine increases the gradient across the valve, and the calculated valve area is unchanged. With pseudo-AS, dobutamine increases the force of contraction and opens the valve, increasing flow. The gradient is unchanged, and so the calculated aortic valve area is increased. an increase in flow opens the valve. Abbreviations: AS: aortic stenosis. AVA: aortic valve area. The velocity-time integrals, which are proportional to the gradients, are depicted in blue.
Exercise stress testing is contraindicated in the presence of critical aortic stenosis. Dipyridamole administration with myocardial perfusion imaging may be used to diagnose myocardial ischemia but does not clarify the severity of aortic stenosis. While exclusion of coronary disease would be necessary before intervention for severe aortic stenosis, this would be done by coronary angiography rather than a myocardial perfusion study. Transesophageal echocardiography can sometimes be used to evaluate the severity of aortic stenosis by planimetry, if the imaging plane is chosen carefully, but is not as good as dobutamine at distinguishing severe stenosis from pseudostenosis and does not provide any information about myocardial contractile reserve.123
An 83-year-old woman presents with pulmonary edema and is intubated for hypoxemic respiratory failure. Point-of-care ultrasonography shows global left ventricular dysfunction and B lines on pulmonary examination suggestive of congestion. She undergoes diuresis, oxygenation improves, and she is extubated successfully. Troponin levels are negative. After extubation, her BP is 102/80 mm Hg, heart rate is 90/min, and respirations are 14/min. Jugular venous pressure is estimated at 12 mm Hg. The amplitude of the carotid pulse feels normal, but the upstroke may be delayed. Lungs show bibasilar rales. Cardiac examination reveals a sustained and nondisplaced point of maximal impulse, a systolic ejection murmur heard best at the left upper sternal border, and an S4 gallop. Full echocardiography with Doppler examination reveals a dilated left ventricle with severe global hypokinesis, an estimated ejection fraction of 20%, and a stroke volume of 30 mL. The aortic valve is calcified, with decreased cuspal excursion, a peak gradient of 25 mm Hg, and a mean gradient of 16 mm Hg.
What test should be performed next?
Links to this note
Footnotes
-
Annabi MS, Touboul E, Dahou A, et al. Dobutamine stress echocardiography for management of low-flow, low-gradient aortic stenosis. J Am Coll Cardiol. 2018;71(5):475-485. PubMed ↩
-
deFilippi CR, Willett DL, Brickner ME, et al. Usefulness of dobutamine echocardiography in distinguishing severe from nonsevere valvular aortic stenosis in patients with depressed left ventricular function and low transvalvular gradients. Am J Cardiol. 1995;75(2):191-194. PubMed ↩