Wilson disease
- related: GI gastroenterology
- tags: #literature #GI
The absence of information pointing to other diagnoses and the pattern of liver function abnormalities seen in this patient make a diagnosis of Wilson disease likely, and abnormalities in copper metabolism would be expected, including a low serum ceruloplasmin (choice A is correct).
Wilson disease is an inherited disorder resulting from mutations in the gene encoding ATPase copper transporting beta (ATP7B), which plays a prominent role in copper metabolism. This enzyme participates in transport of extracellular copper into cells and intracellular transport of copper into the Golgi apparatus, where combination into ceruloplasmin occurs. Diminished ATP7B function causes copper accumulation, particularly in the liver but also in the eye (producing the characteristic Kaiser-Fleischer ring) and the brain (often producing pseudobulbar and motor abnormalities, as well as structural changes seen on MRI). The prominence of either hepatic or central nervous system findings (or both) led to use of the term hepatolenticular degeneration, in addition to the original eponym.
Wilson disease may present at any age, but the vast majority of patients are identified before 50 years old, with many with symptoms emerging in childhood or early adulthood. Presentation as a chronic neurologic disorder or cirrhosis is more common than presentation as ALF. The disease is more common in women than men, as is first presentation with ALF. This patient’s psychiatric symptoms and spasms (possibly extrapyramidal signs) may signal central nervous system involvement. Identification of the causes of ALF is always important, especially since some underlying disorders have specific treatments (such as the treatment of acetaminophen overdose with the antidote N-acetylcysteine) that can recoup hepatic function and viability and avert the need for liver transplantation. This is true of Wilson disease, which can be treated acutely with copper chelators such as penicillamine or trientine. Confirming this genetic disorder will also prompt screening of first-degree relatives.
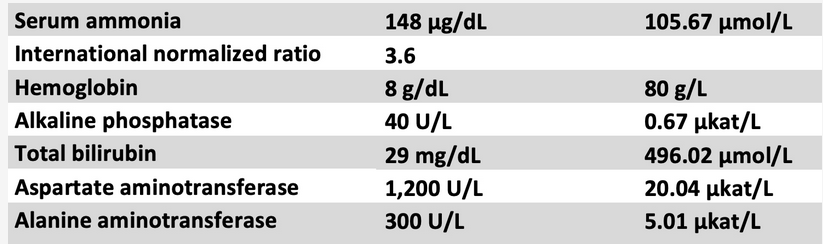
Since Wilson disease is a rare cause of ALF, screening for its presence with simple yet reliable tools would be helpful in patients in whom an earlier diagnosis is absent. In observational studies, analysis of standard test results has been extremely promising in this regard. Specifically, if both an alkaline phosphatase-to-total bilirubin ratio <4 and aspartate aminotransferase-to-alanine aminotransferase ratio >2.2 are present, these findings in combination are close to 100% sensitive and specific for distinguishing Wilson disease from other causes of ALF. These ratios are likely related, in the former instance, to the lack of injury to hepatic duct cells (with minimal or no elevation of alkaline phosphatase levels) coupled to hemolysis (causing very high bilirubin levels) in Wilson disease and, in the second instance, to the pattern of hepatocellular injury unique to Wilson disease. Wilson disease can be further confirmed by identifying a low serum ceruloplasmin level (choice A is correct) and/or increase in urinary copper excretion. In unusual cases, liver biopsy, if possible, may be needed and histologically will demonstrate increased copper levels.
In this patient, repeating a serum acetaminophen level would have no value since there is no history of suicidal attempt or analgesic use and the reliable test has already been performed (choice B is incorrect). GGT is elevated in primary biliary cirrhosis and other liver disease associated with cholestasis, but not in Wilson disease (choice C is incorrect). Viral hepatitis can present as ALF, but cytomegalovirus would be an extremely rare cause of liver injury of this magnitude and would not explain the laboratory patterns seen (choice D is incorrect).1234
A 28-year-old woman is admitted to the ICU with acute liver failure (ALF). She has no significant medical history other than referral for counseling for depression and anxiety in the past year. She also reported to her primary care physician spasm of her lower legs intermittently making it difficult to walk in the past 6 months. She is married and the mother of two healthy children and works full-time as an investment counselor. Four days ago, she felt extremely fatigued with some nausea but no vomiting, and she had a mild headache. She remained home from work. Two days ago, she spent most of the day in bed, and this morning, her husband noted she was lethargic and answered questions very slowly but was still coherent. She was brought to the emergency department, and laboratory testing indicated the presence of liver injury and a coagulopathy. She takes no medications, uses no drugs, and takes no dietary, vitamin, or other supplements.
Some of her notable laboratory tests are shown in Figure 1. Pregnancy test is negative, and serum acetaminophen level is undetectable.
Which of the following serum blood tests is likely to be abnormal and supportive of the underlying cause of this patient’s liver failure?
Links to this note
Footnotes
-
Korman JD, Volenberg I, Balko J, et al; Pediatric and Adult Acute Liver Failure Study Groups. Screening for Wilson disease in acute liver failure: a comparison of currently available diagnostic tests. Hepatology. 2008;48(4):1167-1174. PubMed ↩
-
Roberts EA, Schilsky ML. Current and emerging Issues in Wilson’s disease. N Engl J Med. 2023;389(10):922-938. PubMed ↩
-
Schilsky ML, Roberts EA, Bronstein JM, et al. A multidisciplinary approach to the diagnosis and management of Wilson disease: 2022 Practice Guidance on Wilson disease from the American Association for the Study of Liver Diseases. Hepatology. Published online December 7, 2022. PubMed ↩