WPW is ventricular preexcitation
- related: cardiac arrythmia
- tags: #literature #cardiology
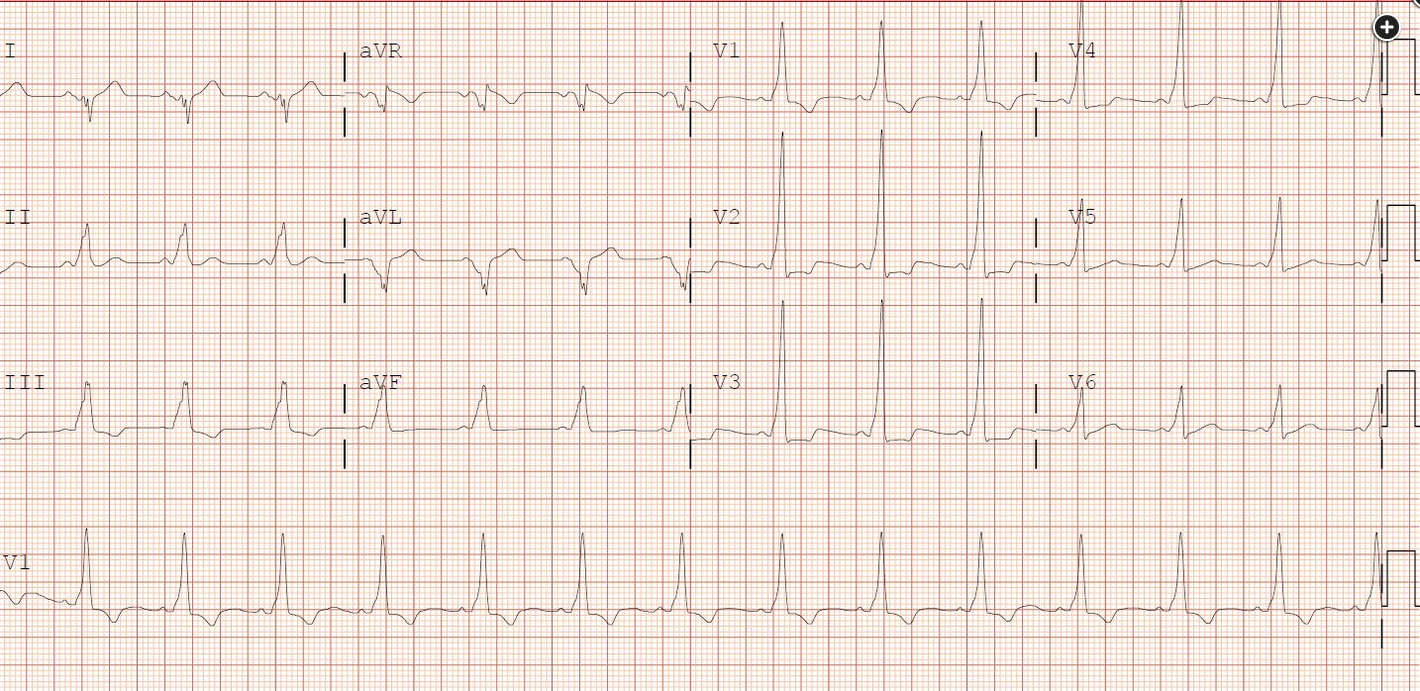
The ECG in Figure 1 demonstrates ventricular preexcitation, signaling an accessory cardiac pathway (choice B is correct).
The terms preexcitation and Wolff-Parkinson-White pattern are often used interchangeably (although the term preexcitation is somewhat broader, as preexcitation can occasionally be due to concealed pathways [eg, in Lown-Ganong-Levine syndrome] that do not produce the Wolff-Parkinson-White pattern). The term Wolff-Parkinson-White syndrome is used when preexcitation is associated with paroxysmal tachyarrhythmias.
Hyperkalemia can cause QRS complex widening, peaked T waves, loss of P waves, fascicular blocks, axis shifts, sine wave appearance, pseudo-ST-elevation myocardial infarction, and Brugada phenocopy (the morphology of ST elevation, primarily in leads V1 and V2, mimicking a Brugada pattern), but does not produce a preexcitation pattern (choice A is incorrect).
Carbon monoxide reduces the oxygen-carrying capacity of hemoglobin but is also a mitochondrial poison, binding to cytochromes and reduced nicotinamide adenine dinucleotide phosphate reductase, impairing oxidative phosphorylation. These properties can cause myocardial stunning or overt myocardial ischemia but do not produce preexcitation (choice C is incorrect). Subendocardial ischemia generally causes ST depression or T-wave inversion but not a preexcitation pattern (choice D is incorrect).
The two dominant ECG features that define preexcitation are shortened PR interval and QRS widening due to delta wave. Preexcitation is uncommon (in <1% of the population) but not rare, and it will occasionally be present in patients critically ill from another cause, as in this patient. Associated tachyarrhythmias (ie, preexcitation syndrome) are quite uncommon, seen in approximately 1% of those with the ECG pattern. Tachyarrhythmias are often bothersome (palpitations, lightheadedness, syncope) but only rarely lethal. Atrial fibrillation can be seen in approximately 20% of those with preexcitation syndrome; if atrial impulses are transmitted along the accessory pathway, ventricular rates exceeding 300/min are possible, which can degenerate into ventricular fibrillation.
Hemodynamically stable patients with symptomatic tachyarrhythmias due to antegrade conduction through the AV node and retrograde conduction through the accessory pathway can be treated with vagal maneuvers or AV nodal blocking agents (adenosine, verapamil, β-blocker). IV procainamide is the preferred drug when there is a wide-complex tachycardia. Those with hemodynamic instability should undergo urgent cardioversion.123
Links to this note
Footnotes
-
Bhatia A, Sra J, Akhtar M. Preexcitation syndromes. Curr Probl Cardiol. 2016;41(3):99-137. PubMed ↩
-
Page RL, Joglar JA, Caldwell MA, et al; Evidence Review Committee Chair. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2016;133(14):e506-e574. PubMed ↩