atrial fibrillation
- related: tachycardia, Arrythmia, Cardiology
- tag: #note
- amiodarone dosing for atrial fibrillation
- bleeding risk may outweigh stroke risk for new onset afib patients in ICU
- anticoagulate new onset afib patients after conversion to sinus rhythm for 4 weeks
- anticoagulate new onset afib patients within 48 hours
epidemiology
- most common sustained arrhythmia
- affect more than 33 million persons worldwide
- Lifetime risk for atrial fibrillation is 25% in patients older than 40 years.
- Incidence is strongly associated with and increases with age.
- 10% of persons older than 80 years.
- fivefold increased risk for stroke
- increased risk for heart failure and dementia
- Among patients aged 55 years and older who have a cryptogenic ischemic neurologic event, such as a stroke or transient ischemic attack, occult intermittent atrial fibrillation is thought to be present in up to 25% of cases, and 30-day ambulatory ECG monitoring is indicated for detection. If 30-day ambulatory monitoring is inconclusive, implantation of a cardiac monitor (loop recorder) is reasonable to optimize detection of silent atrial fibrillation.
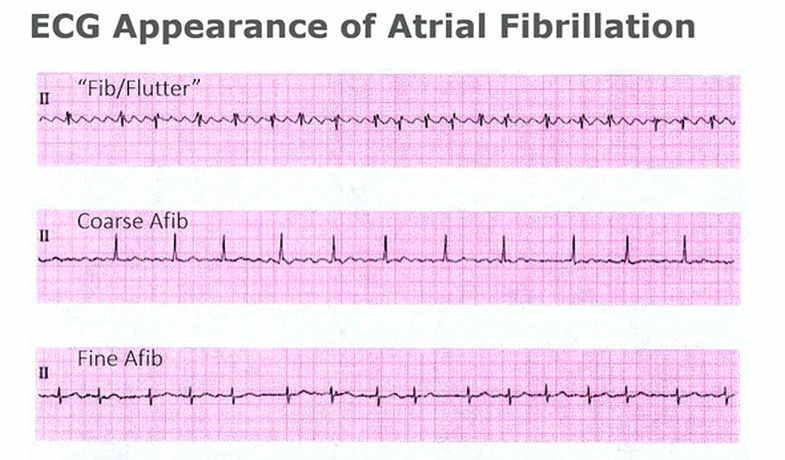
- fib/flutter: manage as afib
- fine afib: nothing on baseline, completely isoelectric
risks
- DM
- obesity
- HTN
- CAD
- HF
- sleep apnea
- smoking
- alcohol consumption
Duration
- paroxysmal: stops within 7 days
- persistent: last for 7 days or more
- long standing persistent: > 1 year
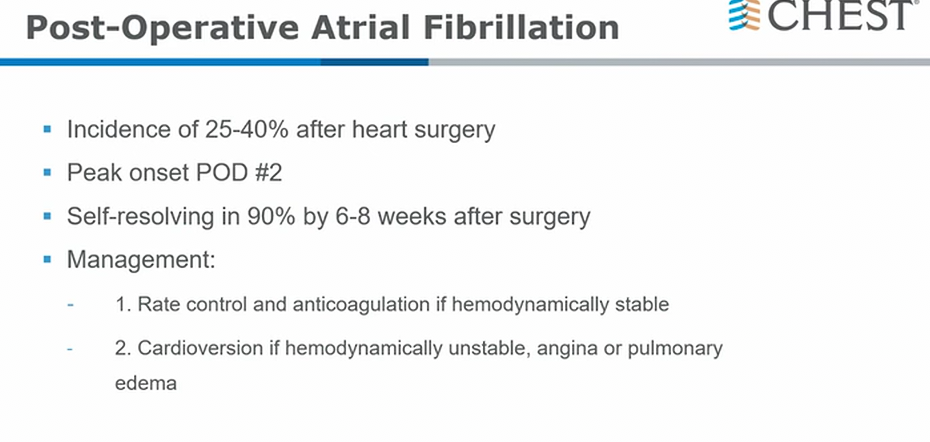
Management
unstable
- synchronized cardioversion: avoids R on T event and Vfib
- unknown duration or > 48 hours duration: initiate AC and continue for 4 weeks at least
stable
- testing
- TSH
- sleep apnea
- echocardiogram for valvular or structural heart disease, left atrial size
Rate control
- goal:
- <60
- <110 in pts without lower EF
Rhythm control
- pill-in-the-pocket approach: pts with infrequent afib and no structural heart disease
- on BB/CCB
- flecainide/propafenone: take at onset of episode
- fleicanide: need AV nodal blockade such as BB to avoid 1:1 Vfib from Afib
- Class 1c: need ischemic work up prior to initiate in hospital. Could also initiate then ischemic work up afterwards
- Class 3: watch out for QTc prolongation (sotalol)
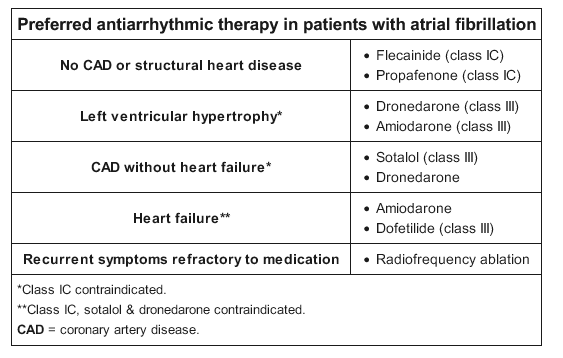
Ablation
- for symptomatic afib despite antiarrythmic
- pulmonary vein isolation
- AV nodal ablation: afib with tachycardia despite rate/rhythm control. Needs permanent pacemaker. Also will remain in afib afterwards and still need AC](##)
cardioversion
- pharm cardioversion: pt without structural heart disease
- can use Ibutilide: monitor on tele for 6 hours or until QTc return to baseline due to small risk of torsades
anticoagulation
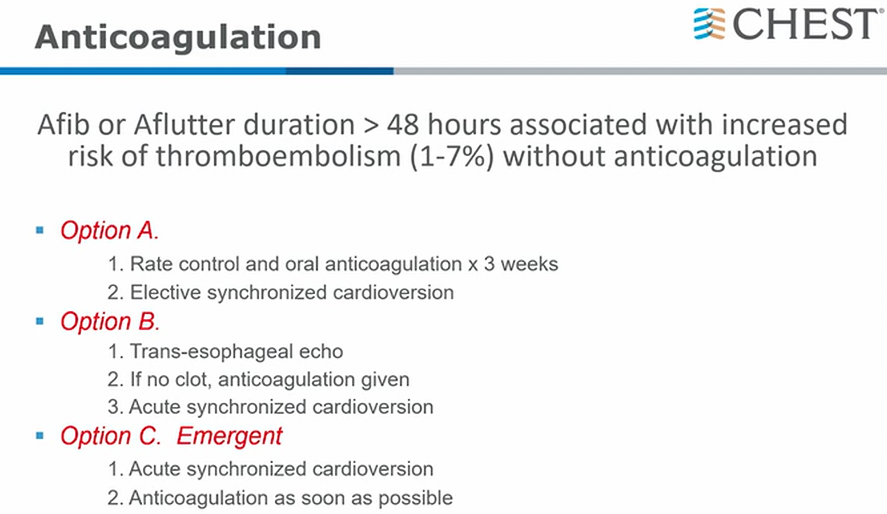
- 48 hours might change to shorter duration in future (e.g. 12 hours)
When to start
- afib duration < 48 hours or low risk for stroke/thrombus
- preprocedural AC for men with chadsvasc more than 1 and women more than 2
- unclear duration or > 48 hours
- AC for 3 weeks before cardioversion
- can use TEE prior to cardioversion
- Continue at least 4 weeks following cardioversion due to increased risk for thrombus formation after sinus rhythm
Valvular vs Nonvalvular
- non-valvular afib: base on CHA2DS2-VASc
- men: AC if score ≥ 2
- women: AC if score ≥ 3
- other valves: aortic valve, MR, TR, mild mitral stenosis
- can use non-vitamin K antagonist (NOAC)
- valvular afib: needs AC
- mechanical prosthesis (mechanical valve replacement)
- moderate to severe MS
- cannot use NOAC, only warfarin
- Pt with HAS-BLED ≥ 3 needs regular evaluation
Agents
- Warfarin
- INR goal 2-3
- NOAC
- kidney/liver function, reevaluate at least annually
- dabigatran: thrombin inhibitor, Pradaxa
- less intracranial bleed
- higher GI bleed
- dyspepsia
- rivaroxaban: 10a inhibitor, Xarelto
- noninferior to warfarin with stroke or embolism
- less intracranial/fatal bleed
- higher GI bleed risk
- apixaban: 10a inhibitor, Eliquis
- superior for stroke prevention
- less major bleed risk
- less intracranial bleed risk
- edoxaban:
- noninferior for stroke prevention
- less major bleed
- reversal agents
- andexanet alfa or 4-factor PCC: for life-threatening bleed 2/2 10a inhibitors
- Idarucizumab: for dabigatran, emergency invasive procedures or life threatening bleeds
- left atrial appendage occlusion: can consider in pt with CHADSVASC ≥ 3
- lower risk for intracranial bleed
- for pts with afib s/p PCI and CHADSVASC ≥ 2
- double therapy: clopidogrel/ticagrelor + AC
- better than triple therapy to reduce risk of bleed
- for pts with afib and stable CAD
- xarelto alone instead ASA + rivaroxaban