candida infections
- related: Pulmonary Diseases, Infectious Disease ID
- tags: #pulmonology #pulmonology
- reason to call ophthalmology in the ICU
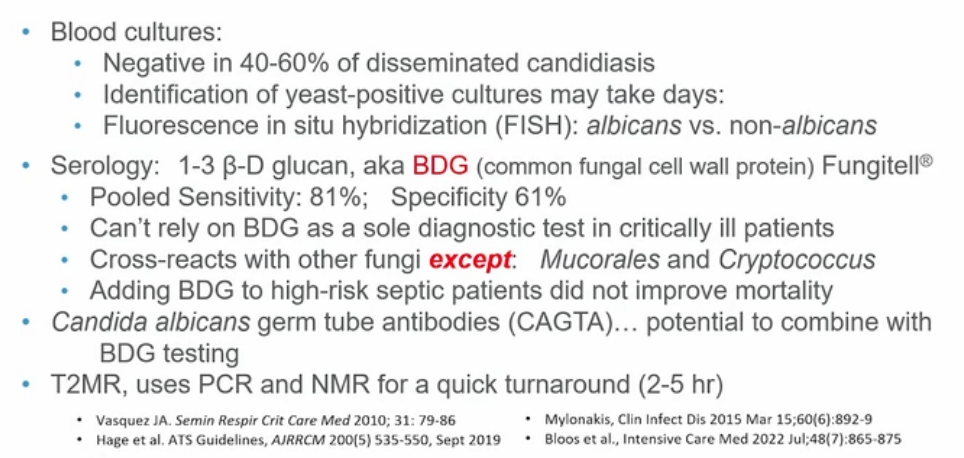
- blood cultures negative so rely on 13BD glucan or fungitell
Lung
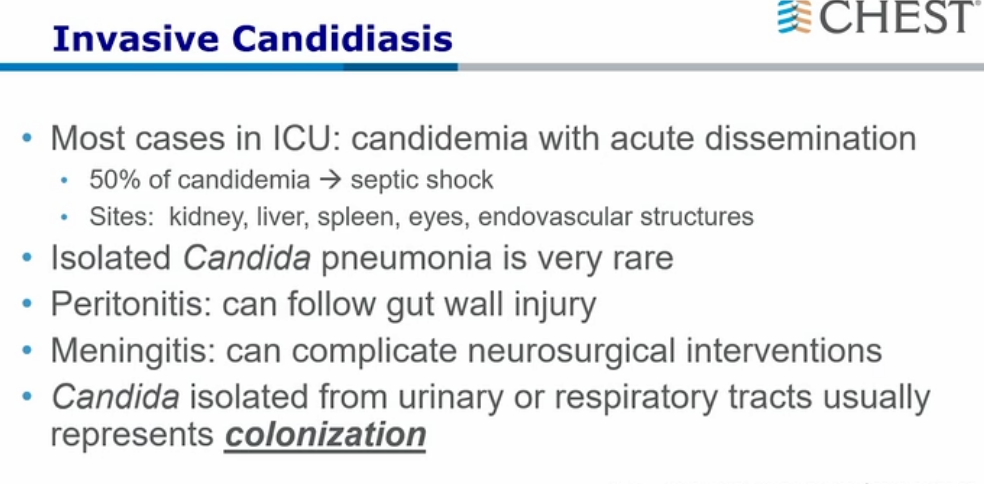
Bronchial tree colonization with Candida species is common in critically ill patients receiving mechanical ventilation, but primary Candida pneumonia and invasive disease are rare. Candida pneumonia is usually not due to aspiration of oropharyngeal secretions but rather to hematogenous spread from disseminated candidiasis (eg, osteomyelitis, septic arthritis, or endocarditis). As a result, diagnosis of Candida pneumonia requires histopathological confirmation.
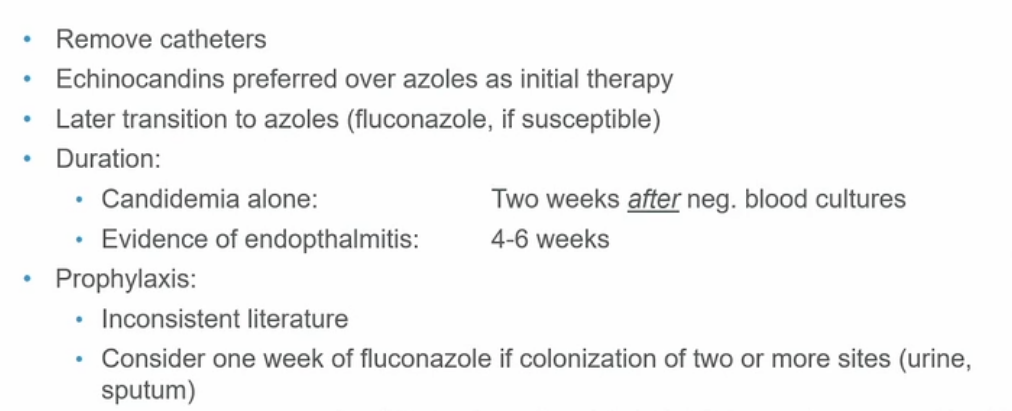
Current guidelines do not recommend antifungal treatment or repeat cultures for immunocompetent patients with Candida from respiratory sputum or bronchoalveolar lavage unless they are immunocompromised. Antifungal treatment is also reserved for immunocompetent patients with a primary Candida infection at another site who develop new pulmonary lesions suspicious for hematogenous spread. Fluconazole is preferred for treating candidemia, but echinocandins (eg, micafungin) are recommended in patients with severe illness or recent azole exposure.
Renal
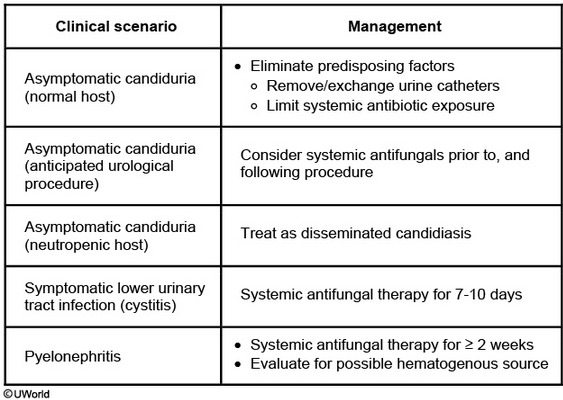
Candida can infect both the upper and lower urinary tract from either an ascending urinary tract infection or a hematogenous source. However, asymptomatic candiduria frequently occurs in patients with chronic urinary catheters likely due to chronic colonization. Current guidelines recommend urinary catheter removal in patients with asymptomatic candiduria or catheter exchange if catheter removal is not possible. Patients with persistent candiduria (especially diabetics) require imaging (e.g., CT or renal ultrasound) after catheter removal/exchange to rule out hydronephrosis, perinephric abscess, or possible fungus ball (rare complication that may require surgical intervention).
Systemic antifungal therapy may lead to antifungal-resistant Candida species and is usually avoided in asymptomatic patients. However, therapy is considered in patients at high-risk for disseminated candidiasis (e.g., adult patients with neutropenia or who are undergoing urologic procedures) (Choices A and B). Symptomatic candiduria (e.g., flank pain, abdominal pain, costovertebral angle tenderness) should be treated with antifungal therapy based on the species of Candida identified, extent of infection, and suspected etiology (e.g., lower urinary tract ascending infection or hematogenous source).
This patient improved after initial treatment for pneumonia and has no symptoms of upper or lower urinary tract infection; he only requires catheter exchange for his candiduria. His catheter might have been placed to avoid contamination of the decubitus ulcer.
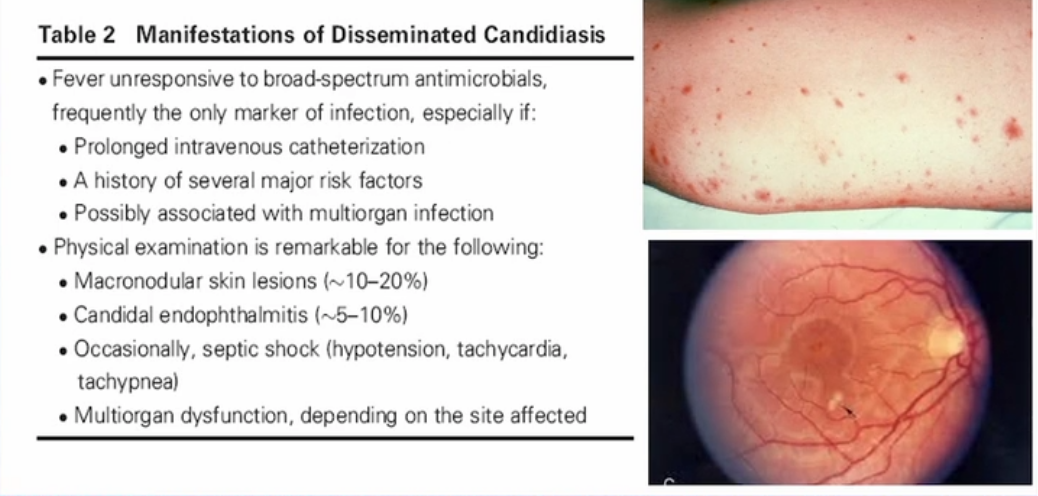
Eye
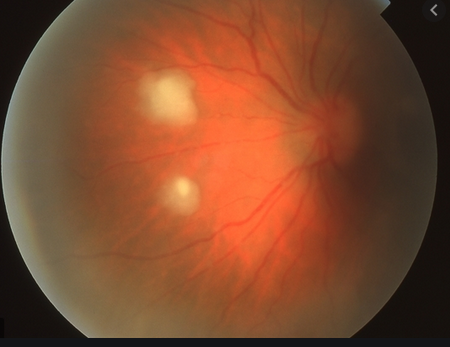
The eye is frequently affected, and patients often have fever, decreased visual acuity, and eye pain. Funduscopic examination typically reveals focal, glistening, white, mound-like lesions on the retina that may extend into the vitreous, with resultant vitreous haze.
Candida endophthalmitis is a vision-threatening infection and must be treated aggressively. Those who have endophthalmitis due to hematologic seeding (as in this case) typically develop chorioretinitis, which can then spread into the vitreous or aqueous.
Patients with vitreous involvement usually require systemic antifungals such as amphotericin B, intravitreal antifungal injection, and vitrectomy (to reduce fungal microabscesses that may be recalcitrant to therapy). Treatment with systemic antifungals for 4-6 weeks is required.
Vaginosis
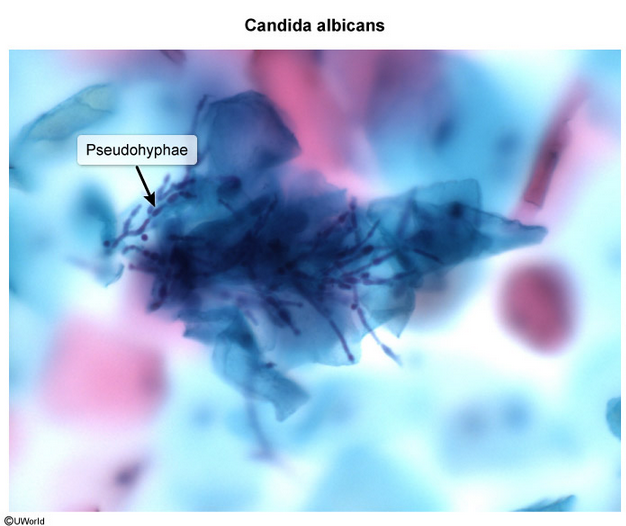
Vulvovaginal candidiasis (VVC) is common because Candida (red arrow) exists as normal vaginal flora. However, overgrowth and invasion of the vaginal cells creates symptomatic VVC, leading to vaginal discharge, pruritus, dysuria, and dyspareunia. Examination findings include vulvovaginal erythema and clumpy white discharge. Pseudohyphae (typically not seen with Candida glabrata) and budding yeast can be visualized on wet-mount microscopy. Potassium hydroxide (KOH) or Gram stain can be added to facilitate visualization of fungal elements. Vaginal culture may be helpful in women with atypical (eg, negative microscopy, mixed vaginitis), severe, or recurrent episodes of VVC.
Treatment of uncomplicated VVC (eg, ≤3 episodes per year, immunocompetent, mild symptoms) is a single course of an oral (eg, fluconazole) or topical (eg, miconazole, clotrimazole) antifungal agent. Complicated infections require longer courses of treatment, and strains other than Candida albicans may be resistant to azoles.