CAR-T and cytokine release syndrome
- related: Oncology
- tags: #literature #hemeonc
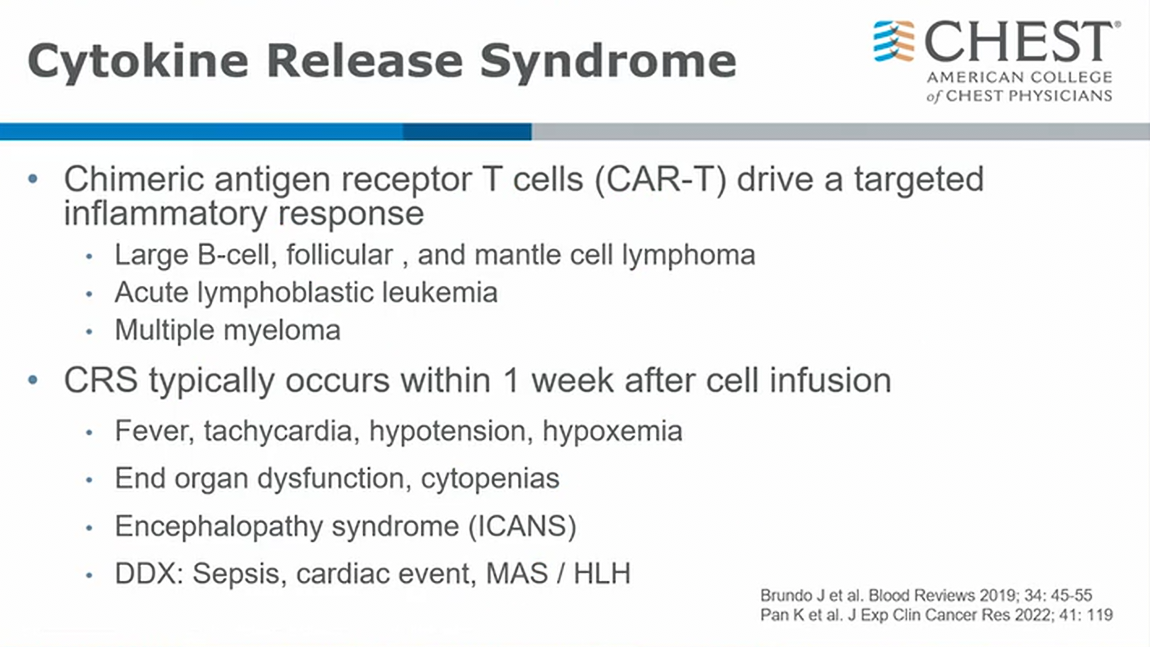
- host immune system activated to attack underlying cancer
- ICANS: CNS mediated inflammatory response
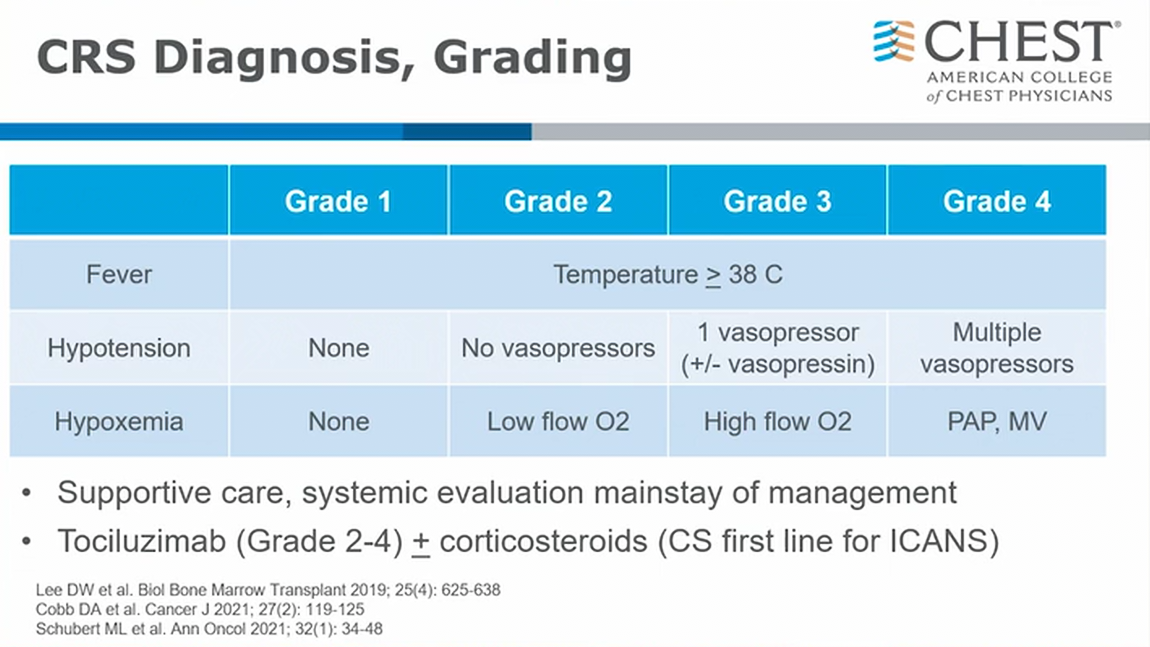
- most important: identify patients who need early therapy
- simple criteria: fever, hypotension, hypoxemia
- ICANS: steroid very effective
- as you suppress immune system, you make CAR-T less likely to work. Consult oncology early.1
CRS is the most common serious toxicity of CAR-T therapy. It is an acute systemic inflammatory response elicited by proinflammatory cytokines released from CAR-T cells that are activated after they have encountered tumor cells. The diagnosis of CRS is made clinically in the correct clinical setting of fever, with or without hypotension, hypoxia, and/or other end-organ dysfunction. Treatment for mild CRS includes supportive care. For more severe CRS cases, such as those in patients with stage 3 or 4 disease and/or requiring admission to the ICU, as in this case, tocilizumab, a monoclonal antibody against the IL-6 receptor, is recommended; for very severe cases, addition of corticosteroids is often recommended. Supportive care alone is insufficient. Despite the often difficult therapeutic course, in general, CRS associated with CAR-T therapy has a good prognosis with treatment.
The differential diagnosis for CRS is broad and includes sepsis, tumor lysis syndrome (TLS), left ventricular dysfunction, heart failure, pulmonary VTE, drug reactions, and disease progression. Although bacteremia can occur in 10% to 30% of patients treated with CAR-T therapy, this patient is on appropriate bacterial coverage for sepsis, they are not absolutely neutropenic, procalcitonin level is normal, 1,3-β-D-glucan and galactomannan tests are negative, and the event is temporally related to the CAR-T therapy; therefore, ongoing sepsis is less likely. The patient is on allopurinol and at medium risk for TLS; nevertheless, even though many laboratories are suggesting that TLS be defined by levels of hyperuricemia, hyperkalemia, hyperphosphatemia, and hypocalcemia, this patient does not meet the standard definition of TLS. In this case, lower extremity venous ultrasound studies are negative, the patient is thrombocytopenic, and they have been on prophylactic heparin; hence, even though the D-dimer value is elevated, it is also an acute phase reactant, so diagnosis of pulmonary embolism is less likely. In addition, bedside point-of-care ultrasound did not note elevated right-sided pressures, and brain-type natriuretic peptide level is only mildly elevated.
Links to this note
-
invasive pulmonary aspergillosis
- The most rapidly progressive and lethal consequence of exposure to Aspergillus spores is invasive aspergillosis, which occurs in patients who are immunosuppressed, with the lung the most commonly recognized site of infection, although dissemination via circulation can occur. Typical settings include patients who are neutropenic undergoing bone marrow transplant, solid organ transplant recipients, and patients undergoing CAR-T cell therapy, especially if it has been complicated by cytokine release syndrome, which requires treatment with tocilizumab and corticosteroids (CAR-T and cytokine release syndrome), as in the patient presented. Invasive aspergillosis has also been described in patients with advanced cirrhosis and after prolonged courses of respiratory failure managed with mechanical ventilation in the ICU, including COVID-19 pneumonitis.
-
CAR-T and ICANS immune effector cell associated neurotoxicity syndrome
- related: Oncology, CAR-T and cytokine release syndrome