CHEST fellow course 2024 Heme Onc Emergencies
- related: Hematology
- tags: #literature #hemeonc
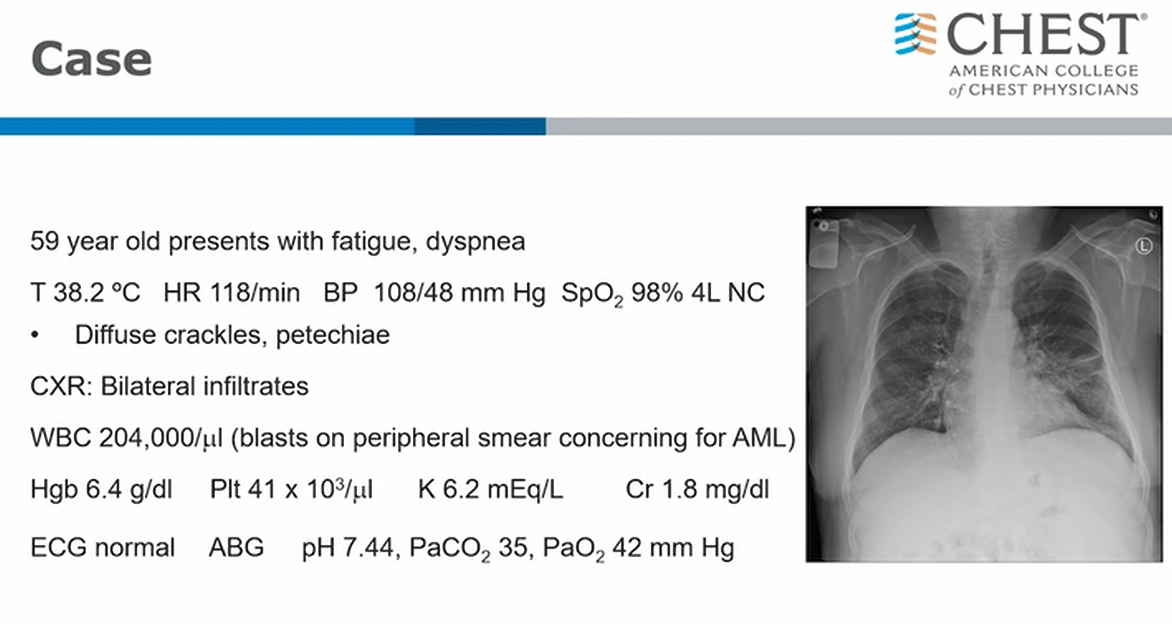
- concerning finding for anemia
- cytopenia
- C
Acute Leukemia
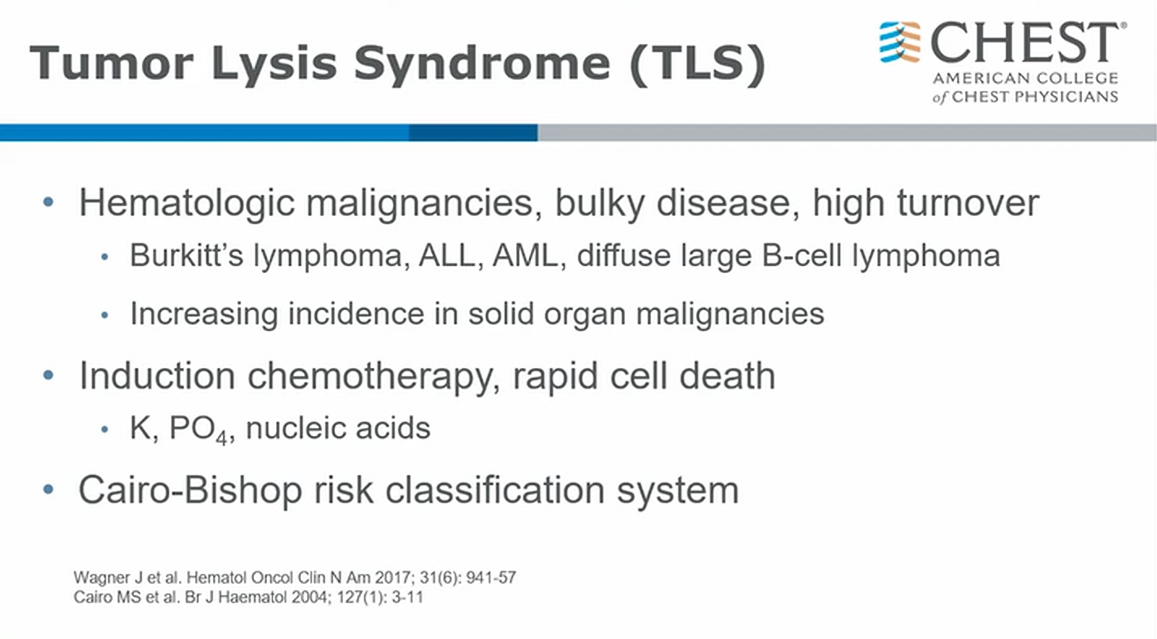
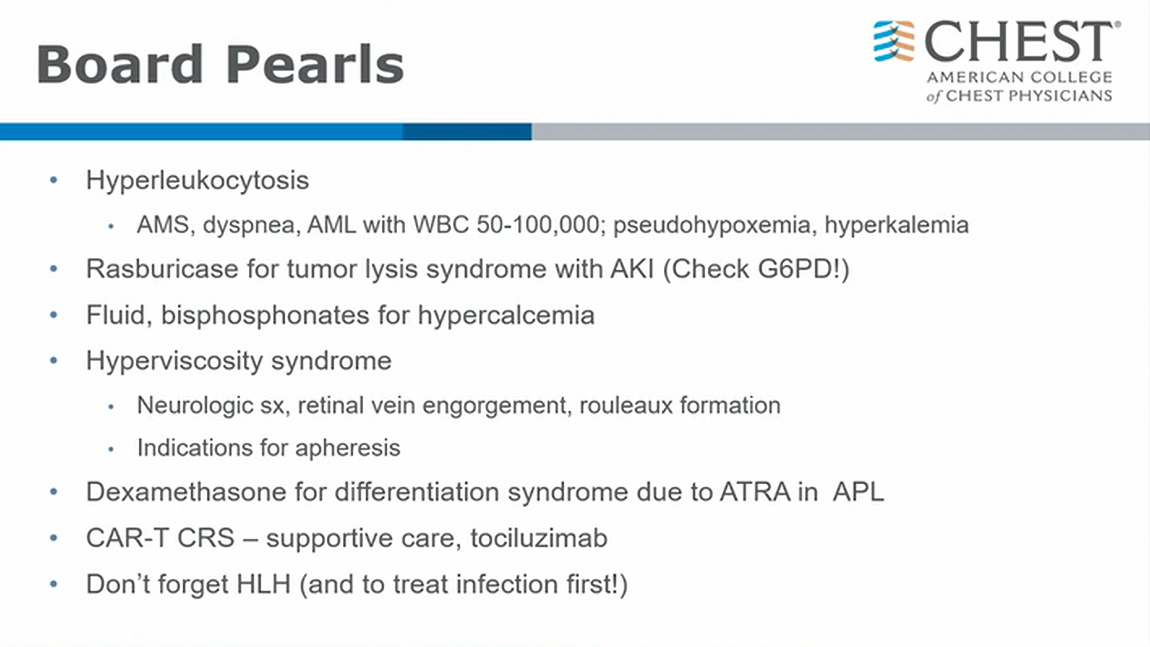
- don’t need to know Cairo scale
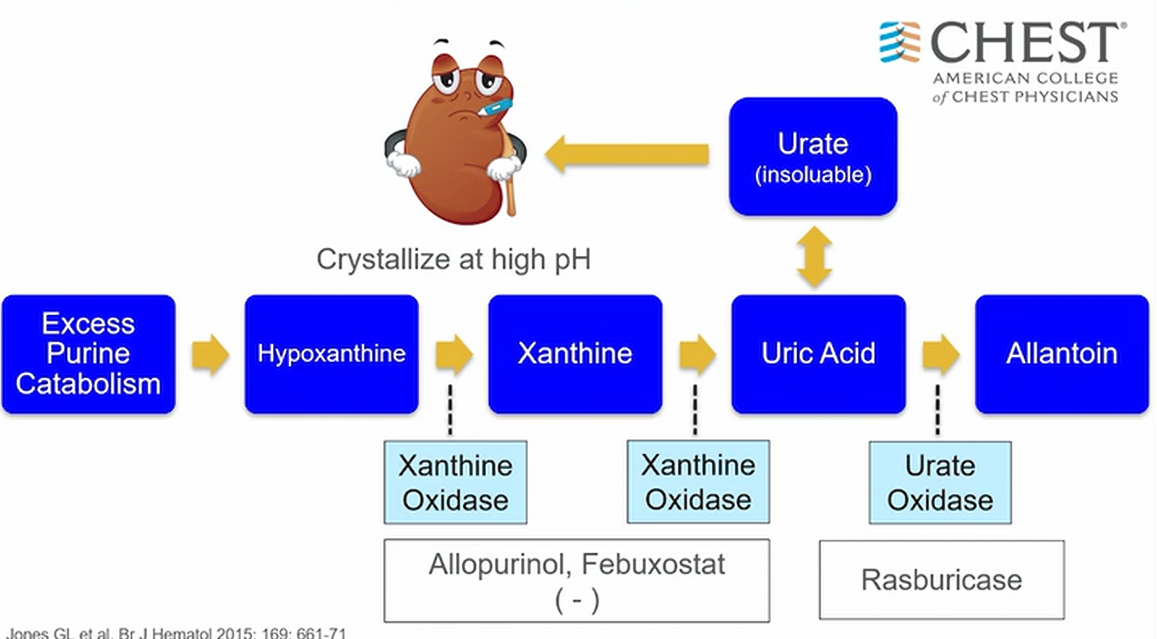
- releasing purine metabolite
- down stream leads to tubular necrosis and AKI
- allopurinol: first line to prevent consequence of TLS
- can cause hypersensitivity reaction: use febuxostat instead
- higher risk of TLS or already have AKI: use rasburicase
- reduces concentration of uric acid
- can actually reverse renal tubular effects from uric acid
- have to check G6PD level
Multiple Myeloma
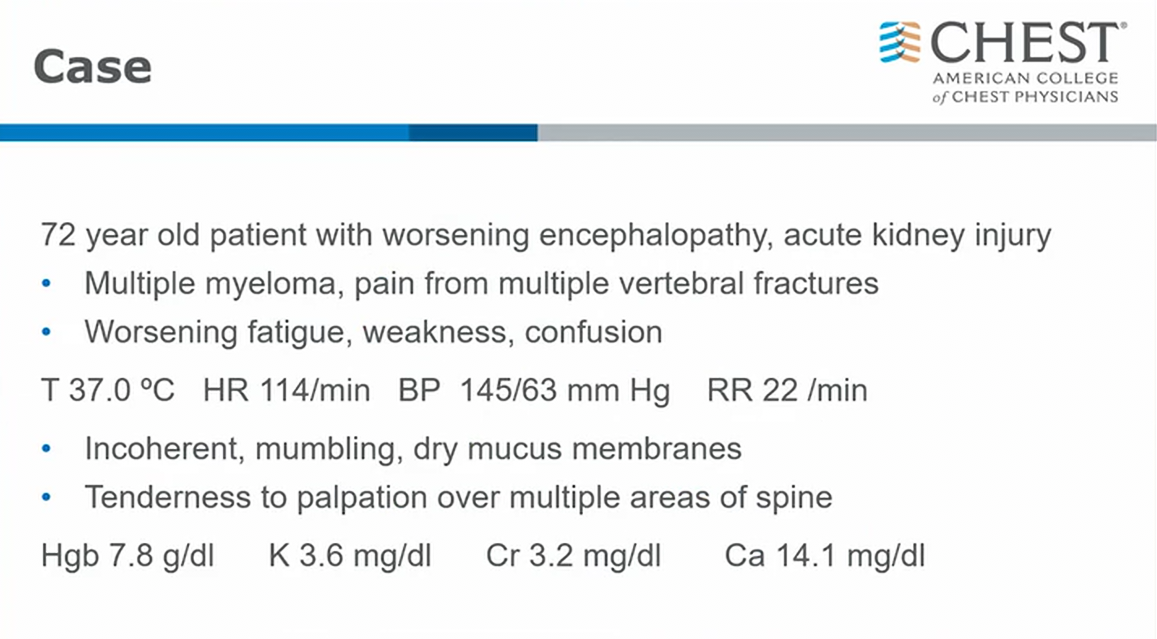
- high Ca
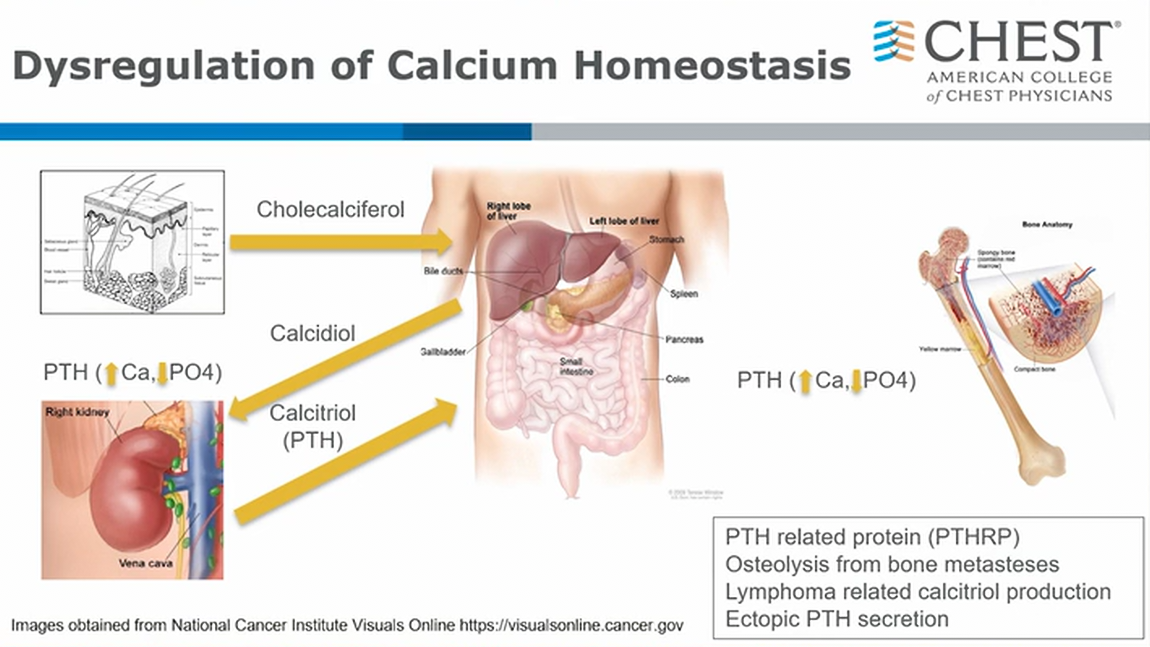
- ingestion, sun exposure, bone osteoclast
- PTHrP: sqCC lung
- bony mets will cause osteolysis such as in MM
- Lymphoma such as Hodgekin’s: peripheral conversion like sarcoid, results in unregulated increase in 1-25 hydroxy vit D
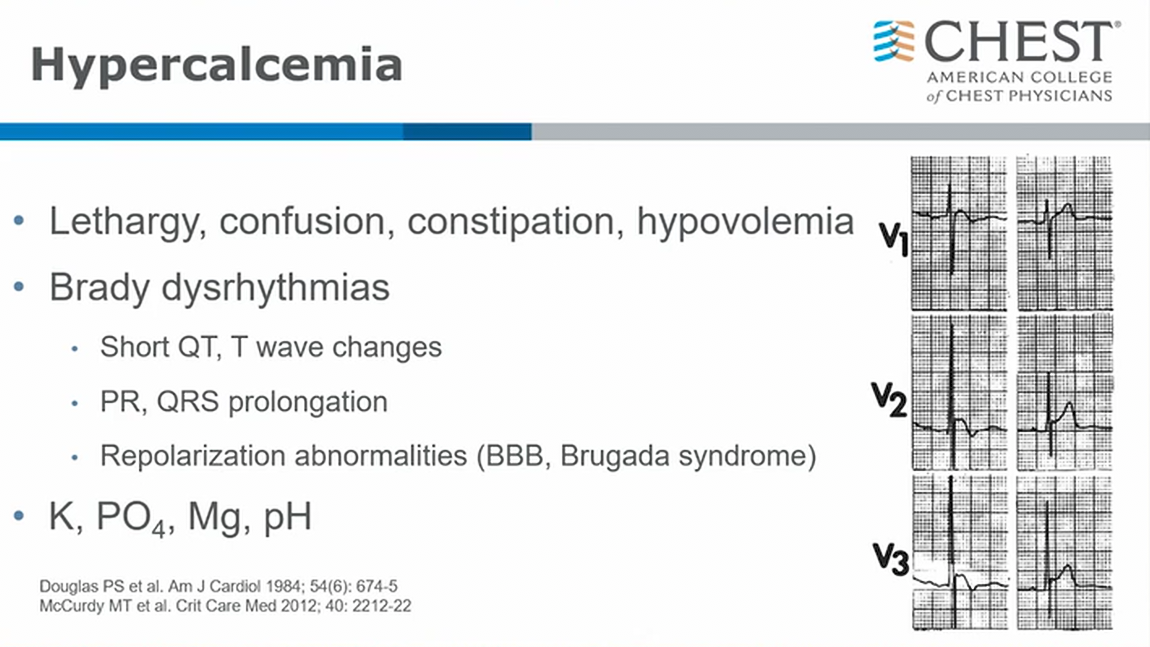
- long PR, QRS, short QT
- end QRS notching like J point for Osborn wave
- pseudo epsilon wave like in Brugada syndrome
- replace phos and mag levels
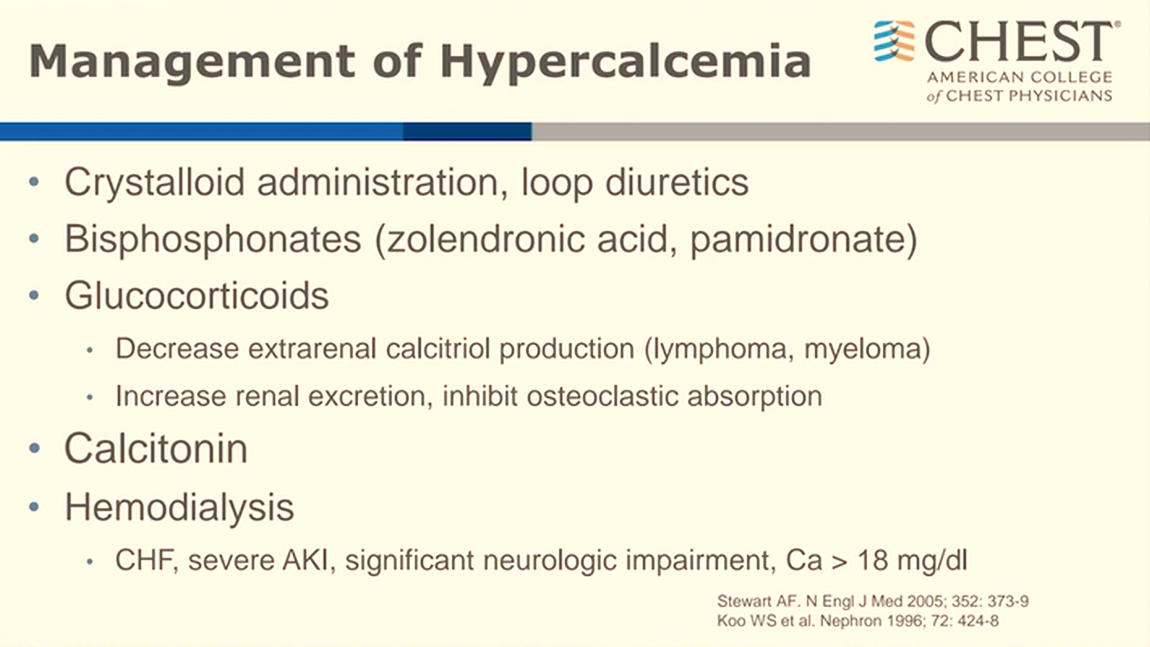
- steroids is good for peripheral conversion of vitamin D
- most of time can get away without dialysis
APML
- happens often
- hypotension
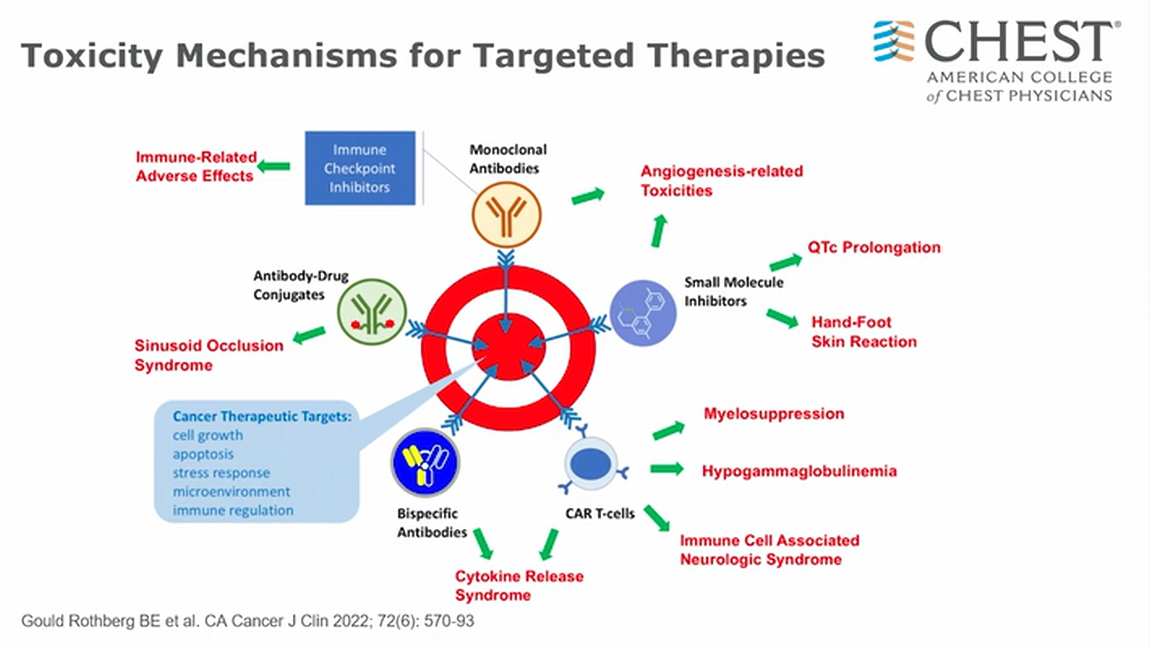
- variety of highly active cancer therapy with side effects
- sinusoid occlusion syndrome: venous occlusive disease (VOD). Most common complication
- angiogenesis related: bleeding
- small molecule inhibitors (kinase inhibitors): QT prolongation and arrythmias
- CAR-T: myleosuppression, cytokine release syndrome
Immune checkpoint inhibitor Pneumonitis
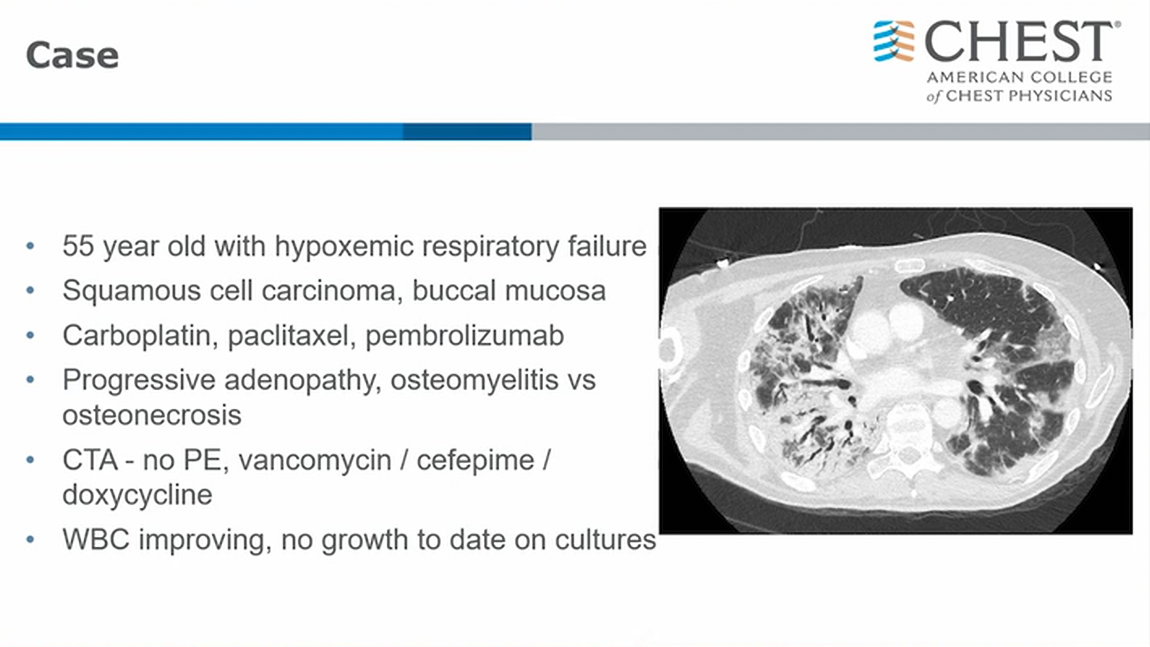
- combination therapy
- concern about deep seated infection
- progressive GGO on L side
- steroids
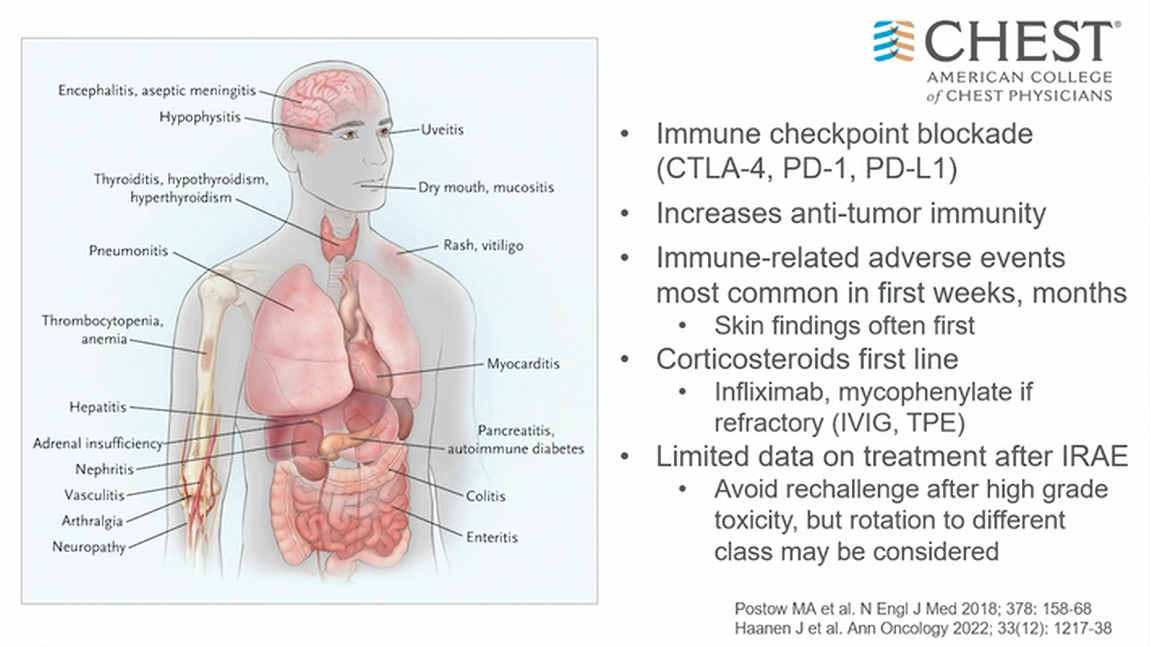
- immune checkpoint inhibitor promotes inflammatory response within first weeks to months
- progressive skin rash: early sign of ICI toxicity
Others
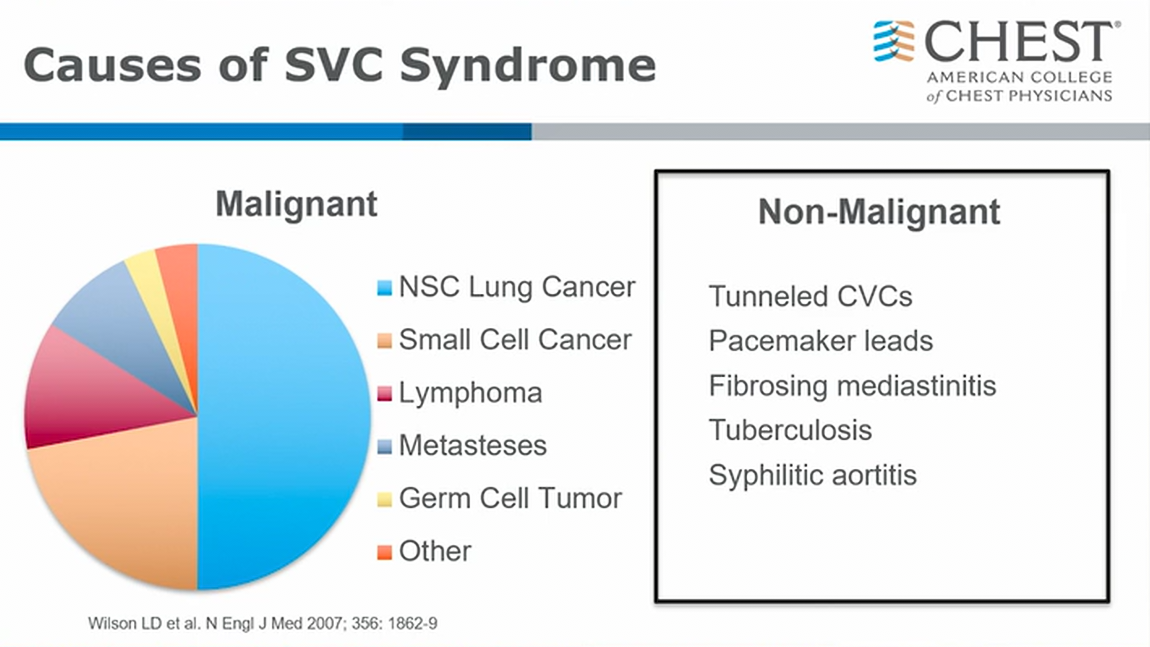
- increase frequency of nonmalignant causes
- histoplasmosis causing fibrosing mediastinitis
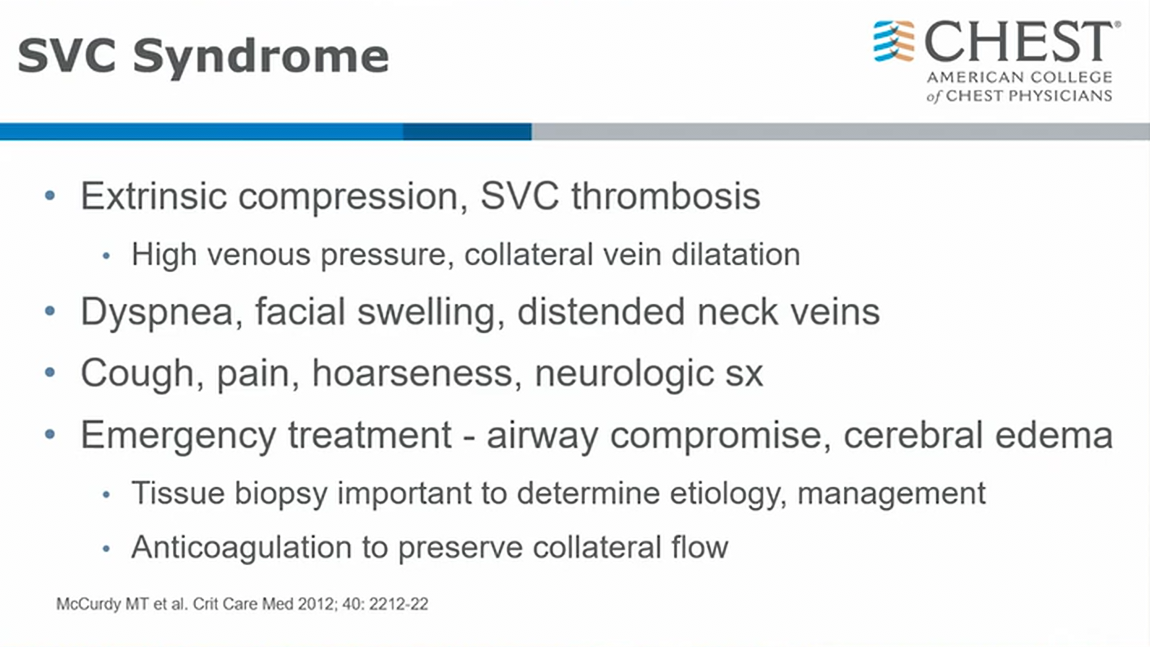
- extrinsic compression and internal involvement of SVC, either tumor/clot
- anticoagulate if no contraindication. Often will rely on venous collaterals flow back to heart (low flow and small diameter, easy to thrombose)
- compression from either fracture or from tumor invasion itself
- medical emergency
- rad onc vs NSY
- MRI better than contrast CT
- 4th ventricle disease (cerebellum and brainstem) have different treatment options
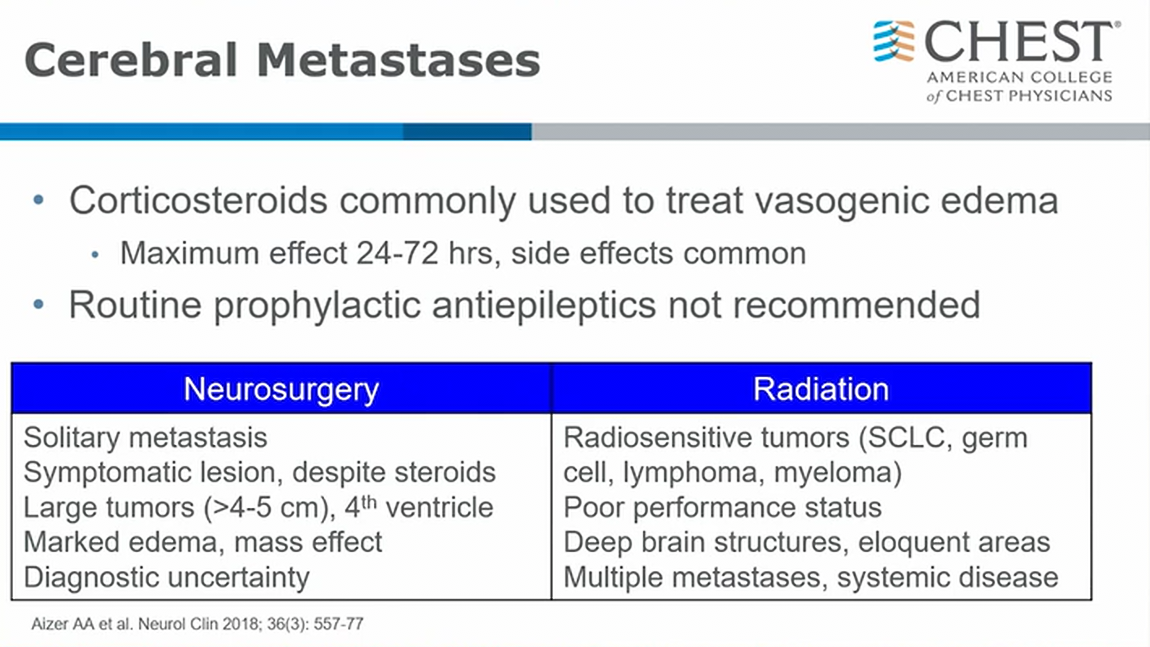
- steroids can buy time for a few days while you look for primary cancer
- infratentorial lesions/cerebellum: smaller space and more poor prognosis => NSY more likely intervention
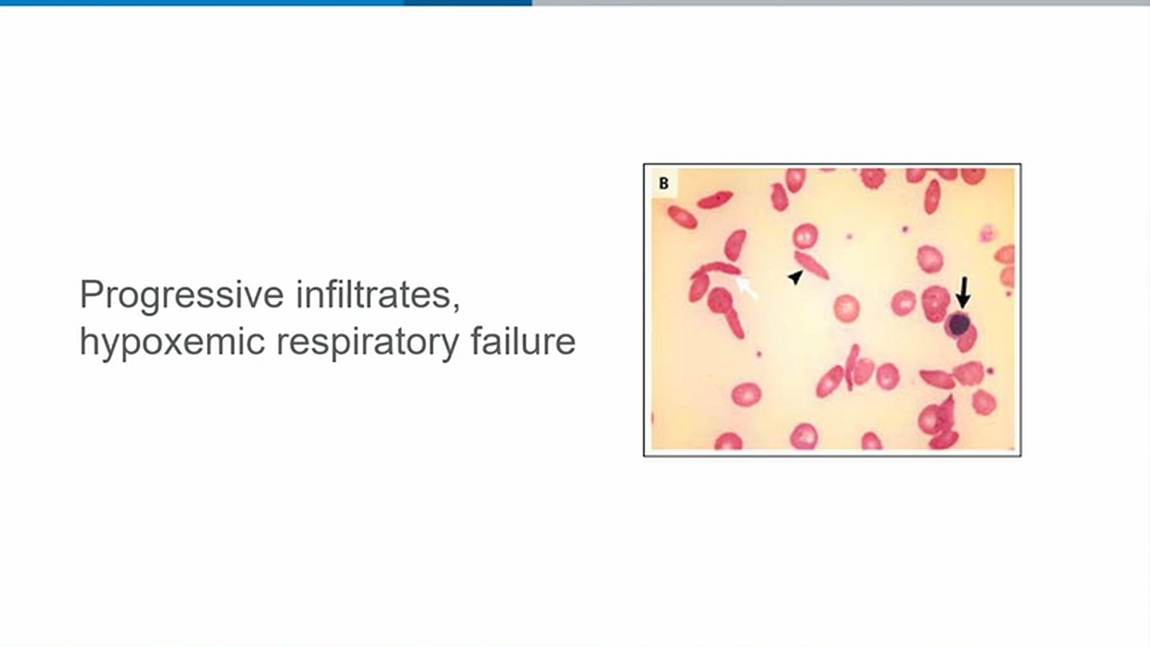
- sickle cell
- acute chest syndrome
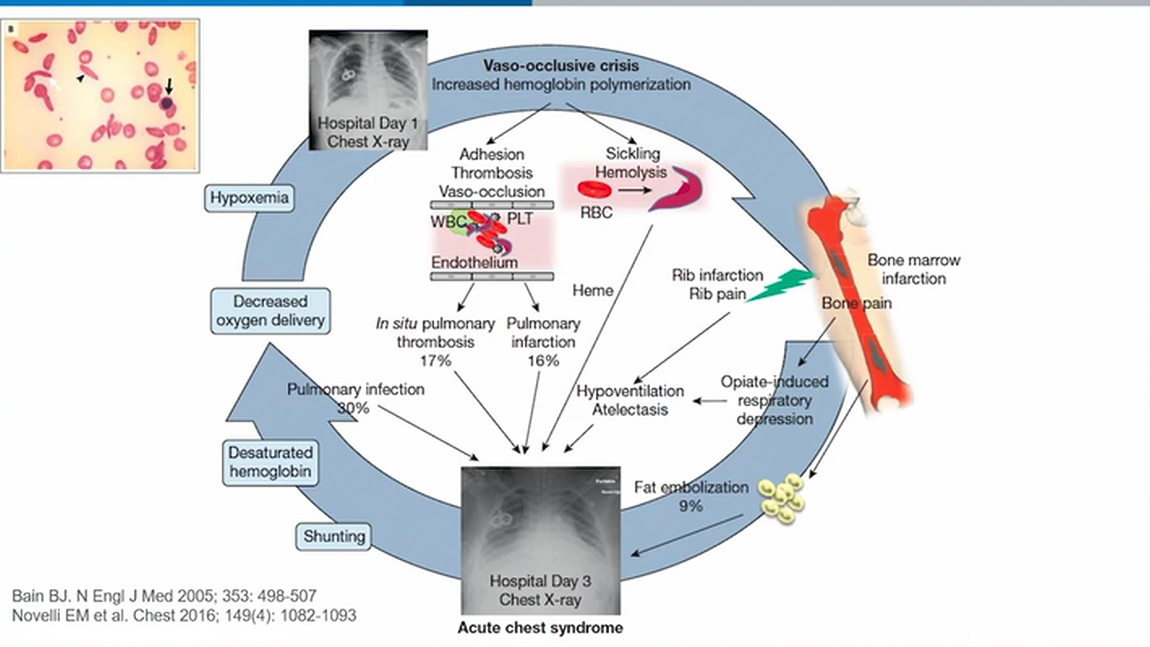
- sludge, thrombosis, release inflammatory mediators, compromise blood flow, in situ pulmonary thrombosis, infarction, inflammation of lung
- bad sickle crisis: bony infarction in ribs. Can’t breath
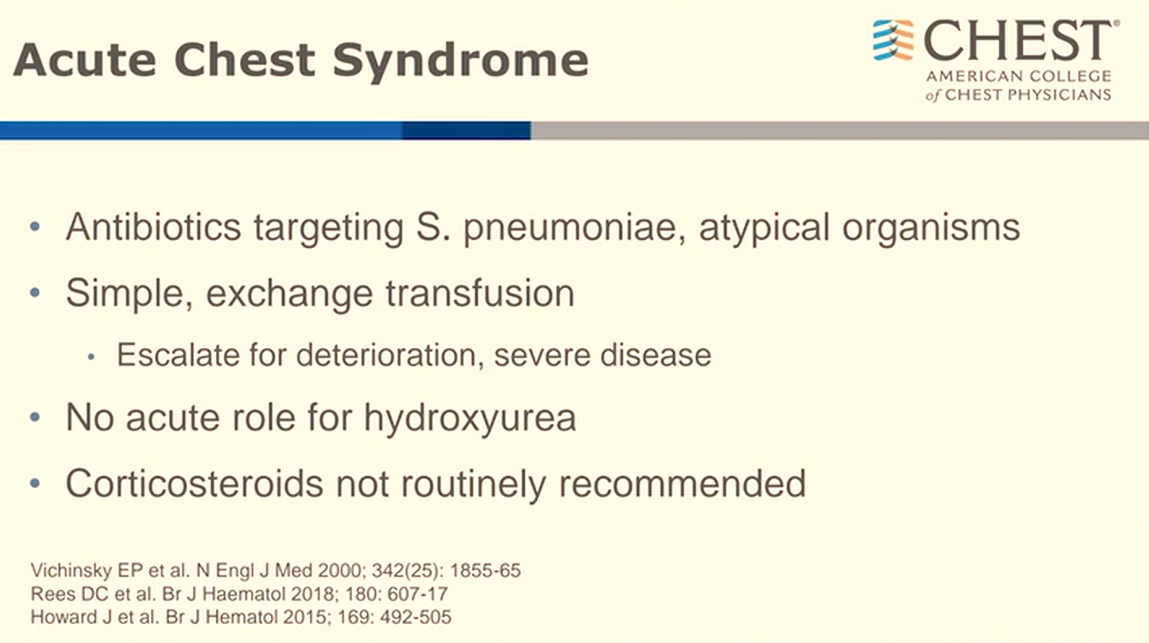
- target encapsulated organisms from functional asplenia
- exchange transfusion. If not, then normal blood for simple volume expansion
- hydroxyurea for chronic for reducing Hgb-F
- steroids used to be used but not anymore: not effective
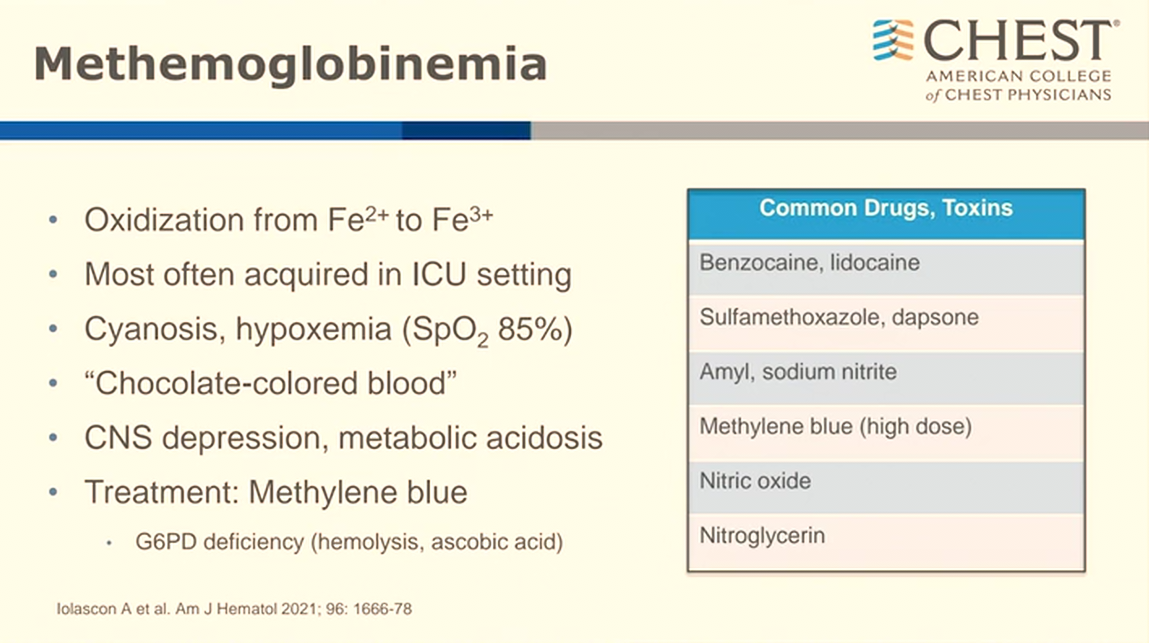
- abruptly cyanotic
- encephalopathy: more worrisome
- most classic: caine and dapsone
- leukopheresis vs apheresis
- no clear mortality benefit of leukopheresis over cytoreduction
Links to this note
-
CAR-T and cytokine release syndrome
- [^1]: CHEST fellow course 2024 Heme Onc Emergencies [^3]: Azoulay É, Castro P, Maamar A, et al; Nine-I investigators. Outcomes in patients treated with chimeric antigen receptor T-cell therapy who were admitted to intensive care (CARTTAS): an international, multicentre, observational cohort study. Lancet Haematol. 2021;8(5):e355-e364. PubMed [^4]: Jones GL, Will A, Jackson GH, et al; British Committee for Standards in Haematology. Guidelines for the management of tumour lysis syndrome in adults and children with haematological malignancies on behalf of the British Committee for Standards in Haematology. Br J Haematol. 2015;169(5):661-671. PubMed [^5]: Outcomes in patients requiring intensive care for CAR T-cell toxicity. Drug Ther Bull. 2021;59(11):166. PubMed [^6]: Shimabukuro-Vornhagen A, Böll B, Schellongowski P, et al. Critical care management of chimeric antigen receptor T-cell therapy recipients. CA Cancer J Clin. 2022;72(1):78-93. PubMed [^7]: Yan Z, Zhang H, Cao J, et al. Characteristics and risk factors of cytokine release syndrome in chimeric antigen receptor T cell treatment. Front Immunol. 2021;12:611366. PubMed
-
tumor lysis syndrome risk is highest in leukemia and lymphomas
-
use allopurinol for prophylaxis and rasburicase for treatment of tumor lysis syndrome
-
acute leukemia and hyperkeukocytosis
- [^1]: CHEST fellow course 2024 Heme Onc Emergencies [^3]: Bewersdorf JP, Zeidan AM. Hyperleukocytosis and leukostasis in acute myeloid leukemia: can a better understanding of the underlying molecular pathophysiology lead to novel treatments? Cells. 2020;9(10):2310. PubMed [^4]: Giammarco S, Chiusolo P, Piccirillo N, et al. Hyperleukocytosis and leukostasis: management of a medical emergency. Expert Rev Hematol. 2017;10(2):147-154. PubMed [^5]: Porcu P, Cripe LD, Ng EW, et al. Hyperleukocytic leukemias and leukostasis: a review of pathophysiology, clinical presentation and management. Leuk Lymphoma. 2000;39(1-2):1-18. PubMed [^6]: Shallis RM, Stahl M, Bewersdorf JP, et al. Leukocytapheresis for patients with acute myeloid leukemia presenting with hyperleukocytosis and leukostasis: a contemporary appraisal of outcomes and benefits. Expert Rev Hematol. 2020;13(5):489-499. PubMed [^7]: Van de Louw A, Desai RJ, Schneider CW, et al. Hypoxemia during extreme hyperleukocytosis: how spurious? Respir Care. 2016;61(1):8-14. PubMed
-
HLH associated with malignancy
- [^1]: CHEST fellow course 2024 Heme Onc Emergencies [^3]: Debaugnies F, Mahadeb B, Ferster A, et al. Performances of the H-score for diagnosis of hemophagocytic lymphohistiocytosis in adult and pediatric patients. Am J Clin Pathol. 2016;145(6):862-870. PubMed [^4]: Fardet L, Galicier L, Lambotte O, et al. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66(9):2613-2620. PubMed [^5]: Hayden A, Park S, Giustini D, et al. Hemophagocytic syndromes (HPSs) including hemophagocytic lymphohistiocytosis (HLH) in adults: a systematic scoping review. Blood Rev. 2016;30(6):411-420. PubMed [^6]: Henter JI, Horne A, Aricó M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124-131. PubMed [^7]: Lehmberg K, Ehl S. Diagnostic evaluation of patients with suspected haemophagocytic lymphohistiocytosis. Br J Haematol. 2013;160(3):275-287. PubMed [^8]: Machowicz R, Janka G, Wiktor-Jedrzejczak W. Similar but not the same: differential diagnosis of HLH and sepsis. Crit Rev Oncol Hematol. 2017;114:1-12. PubMed
-
APML and differentiation syndrome aka retinoic acid syndrome
- [^1]: CHEST fellow course 2024 Heme Onc Emergencies [^3]: Lo-Coco F, Avvisati G, Vignetti M, et al; Gruppo Italiano Malattie Ematologiche dell’Adulto; German-Austrian Acute Myeloid Leukemia Study Group; Study Alliance Leukemia. Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. N Engl J Med. 2013;369(2):111-121. PubMed [^4]: Sanz MA, Montesinos P. How we prevent and treat differentiation syndrome in patients with acute promyelocytic leukemia. Blood. 2014;123(18):2777-2782. PubMed [^5]: Stahl M, Tallman MS. Differentiation syndrome in acute promyelocytic leukaemia. Br J Haematol. 2019;187(2):157-162. PubMed [^6]: SEEK Questionnaires