castleman disease
- related: Pulmonary Diseases
- tags: #literature #pulmonology
The most likely diagnosis is Castleman disease (CD) (choice B is correct), also known as angiofollicular or giant lymph node hyperplasia. The clinical manifestations of CD are heterogeneous, ranging from asymptomatic discrete lymphadenopathy to recurrent episodes of diffuse lymphadenopathy with severe systemic symptoms. CD is classified into three distinct variants based on the number of regions of enlarged lymph nodes with characteristic histopathologic findings as well as the presence or absence herpesvirus 8 (HHV-8). The three main distinct histological variants are the hyaline vascular (HV) type, plasma cell type, and mixed type. CD can occur in a single lymph node station, which is referred to as unicentric CD (UCD). CD involving multicentric lymphadenopathy and inflammatory symptoms is referred to as multicentric (MCD). MCD includes human HHV-8–associated MCD; polyneuropathy, organomegaly, endocrinopathy, M proteins, and skin changes (POEMS)-associated MCD; and HHV-8-negative, or idiopathic MCD (iMCD). The pathogenesis of UCD is poorly understood, though recent evidence suggests that it may be caused in some patients by a clonal expansion of lymph node stromal cells. Although the precise cell type within the lymph node responsible for UCD pathogenesis and producing cytokines has also not been identified, possibilities include follicular dendritic cells, germinal center B cells, and interfollicular plasma cells.
The HV histopathologic subtype is the most common form of UCD, accounting for approximately 70% of patients with CD, and presents equally in men or women. A single node or chain of lymph nodes is typically involved, usually in the mediastinum, but may also occur in the cervical, axillary, or abdominal regions. Patients with UCD are often asymptomatic and come to clinical attention when an enlarged lymph node is noted on physical examination or imaging studies. Systemic symptoms are unusual. Laboratory studies are usually normal in patients with UCD.
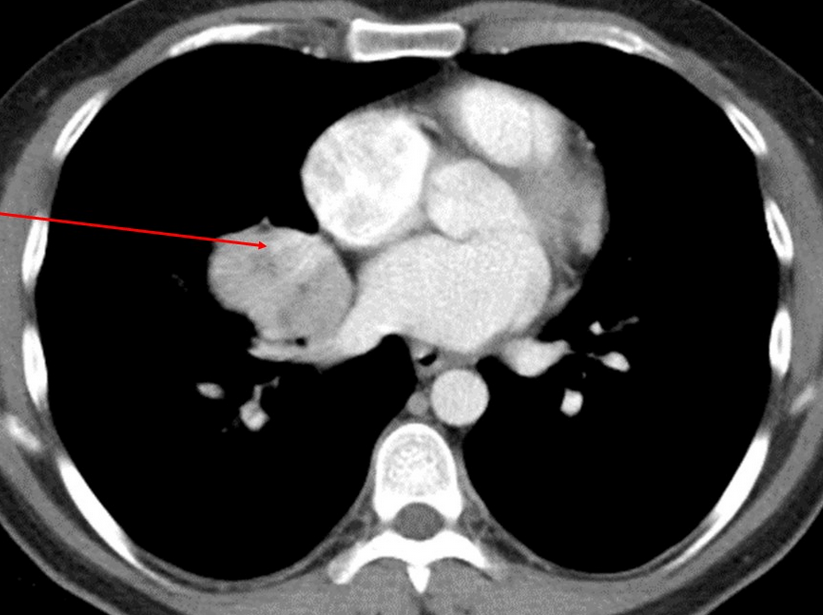
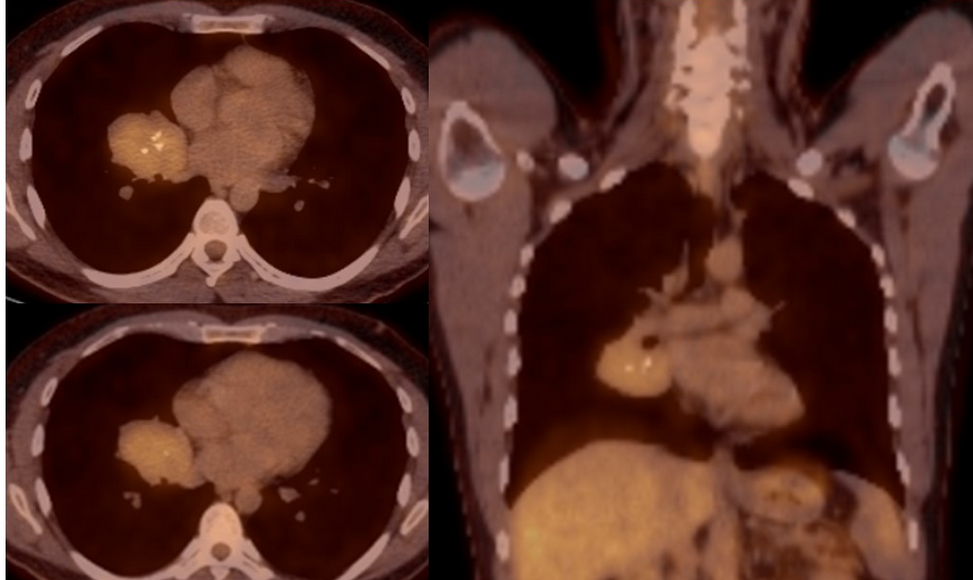
Typically, UCD usually occurs in the mediastinum and hilum and manifests as a rounded solitary mediastinal or hilar mass in asymptomatic patients. On CT imaging, thoracic UCD can manifest in three morphological patterns: a solitary, noninvasive mass (50% of cases); a dominant mass with involvement of contiguous structures (40% of cases); or as matted lymphadenopathy confined to a single mediastinal compartment (10% of cases). Intense contrast enhancement, reflecting hypervascularity of the lesion, is considered to be a CT finding characteristic of UCD (Figure 4). Similar to other inflammatory disease, CD shows mild to moderate fluorodeoxyglucose (FDG) uptake on PET scan, with reported maximum standardized uptake values ranging from 2.93 to 4.5. Histologically, HV-UCD consists of lymph follicles with hyalinization of their walls and concentric whorls of mantle lymphocytes giving an “onion-skin” pattern (Figure 5). Complete surgical resection is almost always curative and is considered the preferred approach for the treatment of UCD.
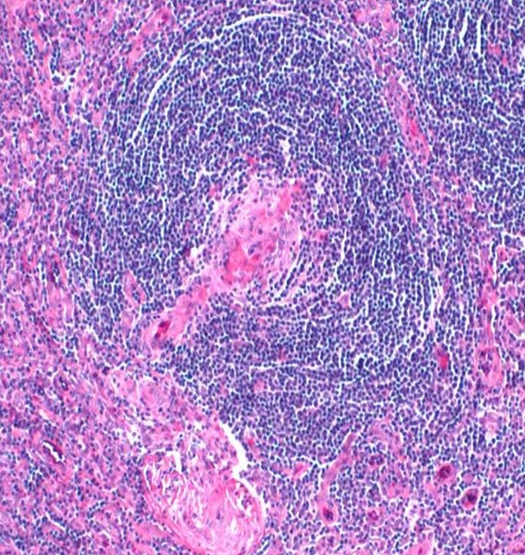
The right lung resection biopsy specimen. Hematoxylin and eosin-stained tissue (×100 magnification) shows lymphoid follicle with hyalinized germinal center with a prominent mantel zone with concentric layering of small lymphocytes in an “onion-skin” pattern.
Although primary pulmonary plasmacytoma, non-Hodgkin lymphoma, and bronchogenic squamous cell carcinoma can all present as a perihilar mass, the histopathological findings, as well as the low FDG-PET avidity, are not consistent (choices A, C, and D are incorrect). These conditions all commonly result in significantly higher FDG-PET avidity, not seen with UCD.1