DRESS syndrome in the ICU
- related: Allergy and Immunology, Dermatology
- tags: #literature #allergy
Causes
Unlike other medication reactions, the onset of symptoms is delayed, often by 2 to 6 weeks, from the time of exposure. Patients begin with fever and flulike symptoms, which are quickly followed by burning skin pain and rash.
Patients typically develop a morbilliform exanthem that starts on the face and upper trunk and spreads distally. Eventually the patients develop striking facial edema and redness (SJS/TEN does not have facial edema), a hallmark of this condition. Oral mucosal involvement is common but is less severe than SJS/TEN or EM major.


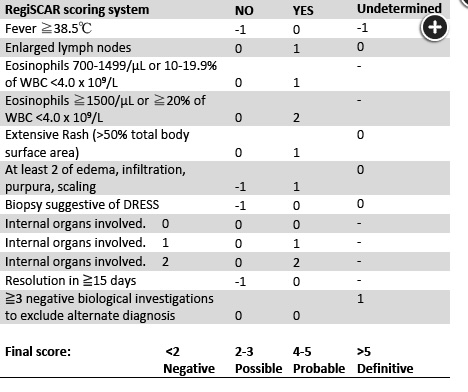
Fever and rash can be complicated to evaluate in the ICU setting. The differential diagnosis can be broad. Outside of a clear history of previous dermatological problems or recent infection (or exposure), medication complications should be considered early in the evaluation. Medication complications are common, although life-threatening complications are uncommon and difficult to evaluate in the setting of critical illness. In this patient, the combination of macular rash, lymphadenopathy, eosinophilia, liver function test abnormalities, and recent changes in antiepileptics strongly suggests the diagnosis of drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome. The RegiSCAR system is a scoring system to help in the diagnosis (Figure 3). This patient’s score is 6.
Discontinuation of the likely offending agent is the first step in managing DRESS syndrome. Levetiracetam is associated with DRESS syndrome. Other antiepileptic medications that are known to cause DRESS syndrome are phenytoin and phenobarbital and clobazam (which the patient is not taking). There are isolated case reports of patients taking divalproex sodium who develop DRESS syndrome, but a clear association has not been made. Baclofen has not been associated with DRESS syndrome. First-line treatment for DRESS syndrome includes systemic steroids but not topical steroids. There are reports of IV immunoglobulin and cyclosporine as second-line agents but not as a first-line therapy.1234
Drug Hypersensitivity Syndrome (or DRESS Syndrome)
Unlike other medication reactions, the onset of symptoms is delayed, often by 2 to 6 weeks, from the time of exposure. Patients begin with fever and flulike symptoms, which are quickly followed by burning skin pain and rash. Patients typically develop a morbilliform exanthem that starts on the face and upper trunk and spreads distally (Figure 131). Eventually the patients develop striking facial edema and redness (SJS/TEN does not have facial edema), a hallmark of this condition. Oral mucosal involvement is common but is less severe than SJS/TEN or EM major.

Generalized morbilliform eruption in a patient with drug reaction with eosinophilia and systemic symptoms (DRESS). Vesicles, blisters, and pustules may also be seen.
Systemic involvement is necessary for the diagnosis and most commonly features eosinophilia (SJS does not have eosinophilia) or an atypical lymphocytosis and elevated transaminase levels. Hypotension, shock, and multisystem organ damage are possible, and death occurs in about 10% of patients. Immediate discontinuation of the causative agent is mandatory, and systemic glucocorticoids tapered over weeks to months can be helpful. DRESS caused by an aromatic antiepileptic agent can also pose a serious threat due to cross-reaction with other aromatic antiepileptics. For example, if phenytoin causes DHS but is appropriately stopped, neither phenobarbital nor carbamazepine should be substituted because of the risk of cross-reaction.
Links to this note
Footnotes
-
Calle AM, Aguirre N, Ardila JC, et al. DRESS syndrome: a literature review and treatment algorithm. World Allergy Organ J. 2023;16(3):100673. PubMed ↩
-
Kardaun SH, Sekula P, Valeyrie-Allanore L, et al; RegiSCAR study group. Drug reaction with eosinophilia and systemic symptoms (DRESS): an original multisystem adverse drug reaction. Results from the prospective RegiSCAR study. Br J Dermatol. 2013;169(5):1071-1080. PubMed ↩
-
Wei BM, Fox LP, Kaffenberger BH, et al. Drug-induced hypersensitivity syndrome / drug reaction with eosinophilia and systemic symptoms. Part I. Epidemiology, pathogenesis, clinicopathological features, and prognosis. J Am Acad Dermatol. 2023:S0190-9622(23)02402-7. PubMed ↩