driving pressure is plateau pressure minus PEEP
- related: ICU intensive care unit
- tags: #literature #pulmonology #icu
Driving pressure (DP) is the pressure required to tidally distend and inflate the alveolar structures. It is a static measurement (plateau pressure minus PEEP) that reflects only compliance properties of the respiratory system during tidal breath delivery, not flow resistive properties. Mathematically, DP is tidal volume/compliance (Vt/C).
Excessive tidal stretch (strain) of alveolar structures during mechanical ventilation can produce ventilator-induced lung injury (VILI). A practical way to address this is the use of “normal” tidal volumes based on ideal lung size (ie, 5-7 mL/kg IBW). However, this may be too simplistic in lungs with extensive regional consolidation. Under these conditions, the volume of lung capable of being ventilated may be markedly reduced (“baby lungs”). Thus, delivery of a normal-sized Vt based on IBW may produce excessive regional tidal stretch in the reduced functional lung. Because compliance may be considered a surrogate for functional lung size, DP has been proposed as a tool to more appropriately scale Vt.
A threshold for a “safe” DP is not clear. Retrospective analyses of multiple randomized clinical trials (most of which were evaluating PEEP strategies, not Vt settings) have suggested that DP values <15 cm H2O seem safer than higher values. Recommendations to keep DP below this threshold have been made by several authorities. In our patient, the DP is 29 (plateau pressure) – 12 (PEEP) or 17 cm H2O. Given the choices offered, the only way to reduce the DP would be to reduce the Vt (choice A is correct; choice D is incorrect).1
Another way to perhaps reduce DP in our patient might be to improve compliance with small, sequential increases or decreases in PEEP. A novel way to assess this is to measure a stress index.
Driving pressure is the difference between maximum and minimum transpulmonary pressure, reflecting cyclic tidal stress. Generally, driving pressure is calculated as the tidal excursion in airway pressure measured at points of zero flow (end-inspiratory and end-expiratory occlusion). Several cautions are in order when attempting to estimate driving pressure. First, even in a passive patient, the set PEEP may not equal the end-expiratory alveolar pressure due to autoPEEP or airway closure. Secondly, peak airway pressure may not equal maximal alveolar pressure since inspiratory flow often does not cease at end inspiration, especially when inspiratory time is short. Finally, calculations of driving pressure assume that pleural pressure does not change significantly: This may not hold, especially when patient effort is high. Studies examining the correlation between driving pressure and outcomes generally assume that patients are passive, that autoPEEP is not present, and that plateau airway pressures are documented accurately.
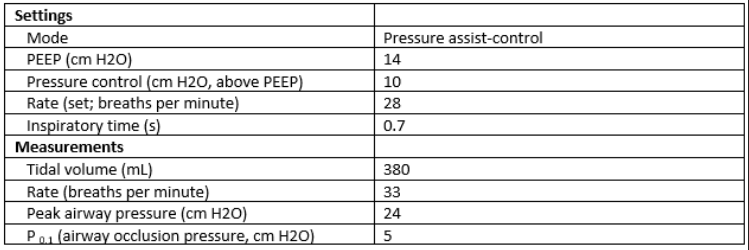
From the information provided in this case, the patient is actively breathing; measured respiratory rate is above the set rate and P0.1 is very high. Substantial inspiratory effort, signaled by the high occlusion pressure, could easily produce a high and variable driving pressure. This pressure may vary substantially from the difference between peak airway pressure and the set PEEP, so that driving pressure is indeterminate (choice C is correct).
It is possible for driving pressure to be less than the level of pressure control (peak airway pressure minus PEEP), especially when there is airflow obstruction. In this case, a driving pressure less than 7 is unlikely (choice A is incorrect).
If end-inspiratory flow was zero (or very low), no patient effort was present, and there was no autoPEEP, peak airway pressure (24 cm H2O) minus PEEP (14 H2O) would be a good estimate of driving pressure (10 H2O).
These conditions are not present in this case (choice B is incorrect). With substantial patient effort, driving pressure greater than 26 could be present in this case, but the information needed to demonstrate this (pleural pressure, plateau airway pressure) is not given (choice D is incorrect).
Driving pressure has been linked to mortality in ARDS, leading to the hypothesis that reducing it below a dangerous threshold could improve outcomes. Limitations in estimating driving pressure retrospectively make any conclusions tentative. Prospective trials will be necessary to learn whether measurement and manipulation of driving pressure affect clinical outcomes.