DVT and PE
- related: Hematology
- tags: #hemeonc
It is unusual for an otherwise healthy 37-year-old to suddenly develop a DVT, especially in the absence of any recent provoking factors such as trauma, surgery, or a long plane trip. The sudden death of this patient's paternal uncle at a young age should raise a red flag that he may have an inherited hypercoagulable condition. The most common cause of inherited thrombophilia (accounting for approximately 50% of cases) is Factor V Leiden, the presence of which results in a resistance to the antithrombotic effects of protein C. Confirming a diagnosis of inherited thrombophilia is extremely important because these patients have an increased risk of developing DVTs, pulmonary emboli, and blood clots in other locations. As a result, they may need to be placed on lifelong anticoagulation.
A prothrombin gene mutation (G20210A) is a common cause of inherited thrombophilia, but it does not necessarily result in a higher level of the protein.
Protein S helps to block coagulation and deficiency of it can lead to thrombophilia. Inherited protein S deficiency is rare compared to the frequency of Factor V Leiden. Antithrombin III deficiency is a relatively rare cause of inherited thrombophilia. Abnormalities in the quantity or functioning of fibrinogen can lead to either bleeding or clotting disorders. However, Factor V Leiden is a more common cause of inherited thrombophilia.
Fat Emboli
Early immobilization and operative fixation of fractures reduces the chances of fat embolism. Supportive care is the mainstay of therapy for clinically apparent fat embolism.
There is no evidence that prophylactic heparin reduces the risk of fat embolism. The use of corticosteroid prophylaxis is controversial, largely because it is difficult to definitively prove its efficacy in a condition with a low incidence, unclear risk factors, low mortality, and a good outcome with conservative management.
DVT
Links to this note
- Hematology
- Cardiology
- aspirin can be used for prophylaxis after treatment of unprovoked recurrent DVT
- related: DVT and PE
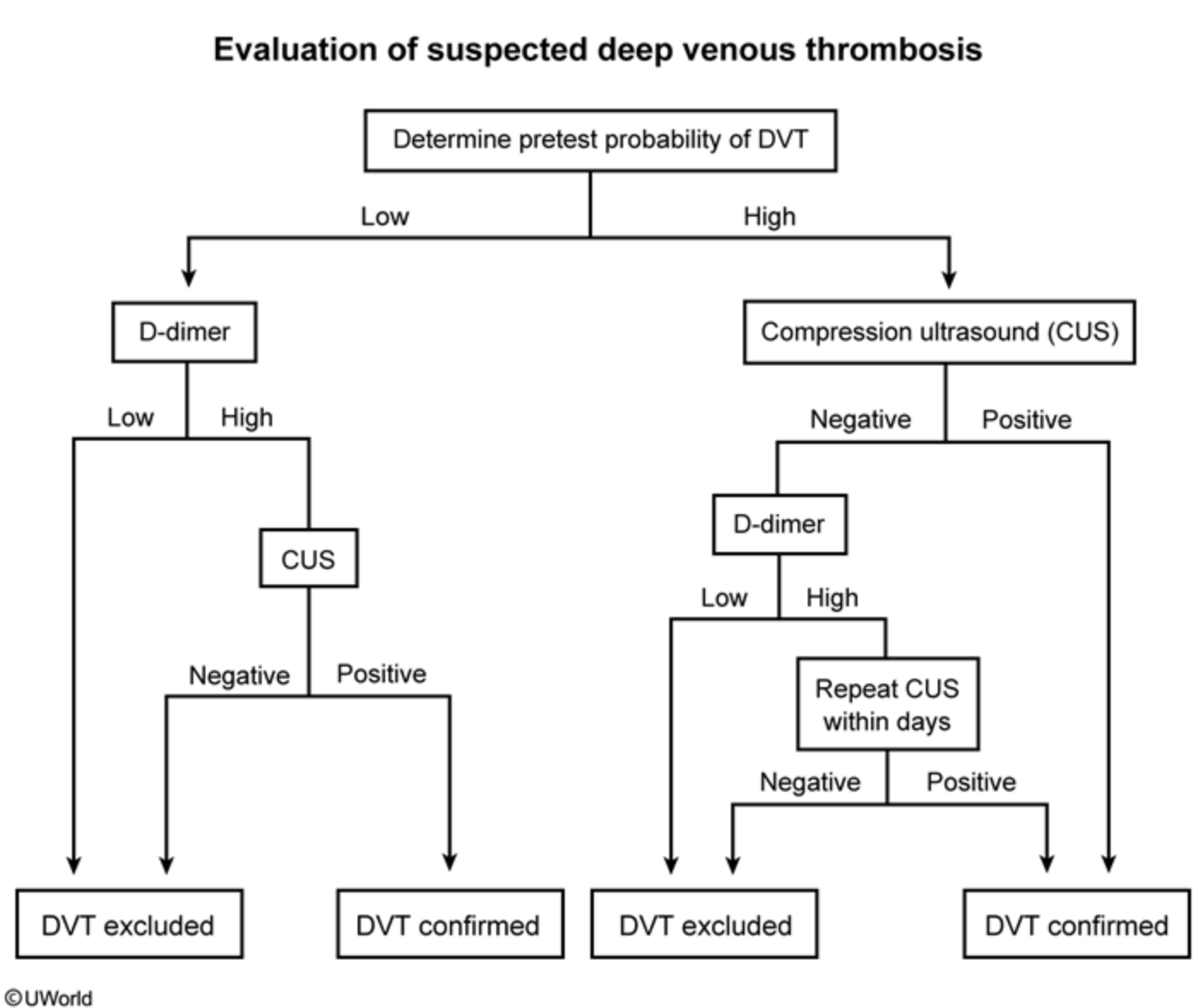
Although not enough clinical information is provided to assess this patient's modified Wells score, her recent long air flight, new-onset unilateral leg edema/pain, and positive Homan sign (pain in the calf on dorsiflexion of the foot) suggest a high pretest probability for deep venous thrombosis (DVT). Negative US with positive D Dimer: repeat US in days.
Patients with suspected DVT are evaluated based on pretest probability as follows:
- Low probability – Obtain moderateor high-sensitivity d-dimer level. A normal d-dimer rules out DVT (d-dimer has a sensitivity of up to 96% but specificity is low); an elevated d-dimer necessitates further evaluation with compression ultrasonography (CUS).
- High probability – Proceed directly to CUS, which has a diagnostic sensitivity of >97% for DVT. As false negatives can occasionally (<3%) occur, patients with a high pretest probability of DVT who have negative CUS testing, continue to be symptomatic, have no clear alternate diagnosis, and have an elevated d-dimer should have repeat CUS within days Patients with moderate pretest probability can be initially evaluated with either high sensitivity d-dimer (normal rules out; elevated requires CUS) or CUS.