epsilon wave on EKG is arrhythmogenic right ventricular cardiomyopathy
- related: ECG samples
- tags: #literature #cardiology
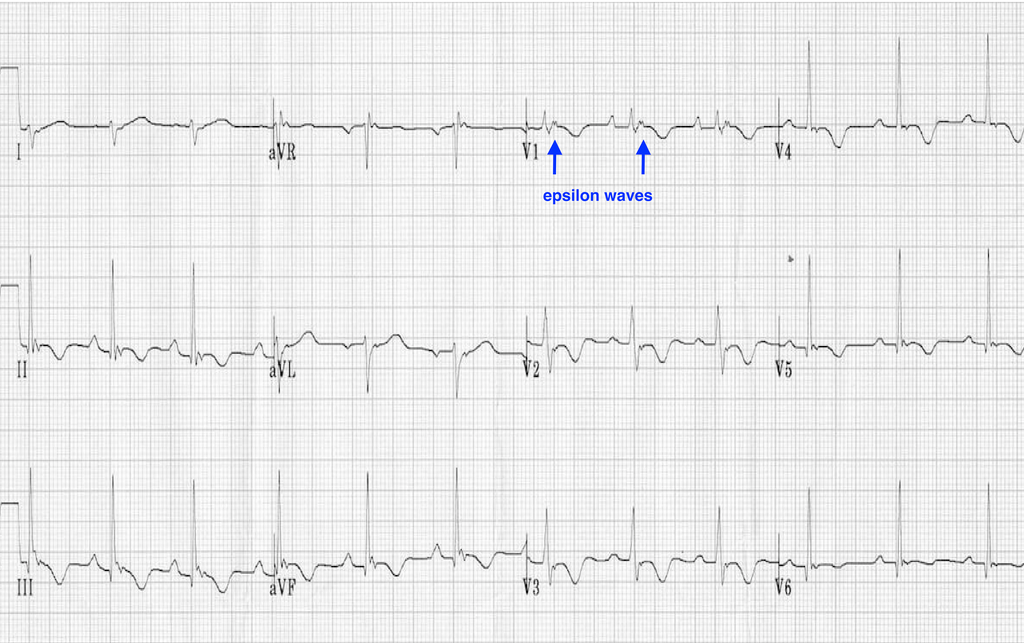
ECG shows T-wave inversions in the anterior precordial leads and a small positive deflection at the end of the QRS complex called an epsilon wave (arrows in Figure 2), both characteristic of arrhythmogenic right ventricular cardiomyopathy (ARVC) (choice B is correct).
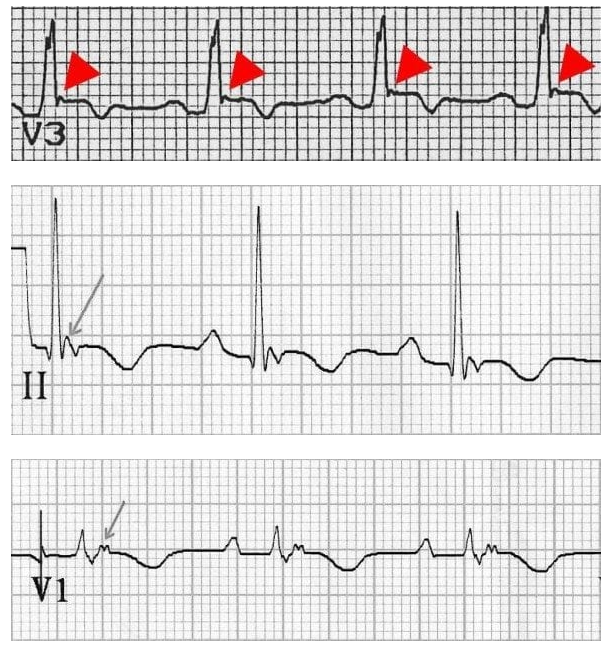
- small blip at end of QRS
- mostly from delay in excitation in RV myocytes1
This disease is heritable (history of a single-car motor vehicle collision in a family member suggests the possibility of sudden cardiac death) and usually results from mutations in genes encoding desmosomal proteins. Presentation is most common between 10 and 50 years old, with palpitations and syncope as common presenting manifestations; ventricular arrhythmias during exercise are typical, as in this case. Sudden death as an initial manifestation is less common, but men and patients with multiple mutations tend to have more severe courses. Genetic screening of first-degree relatives is appropriate.
Definitive diagnosis is made by cardiac MRI showing fibrous or fibrofatty replacement of the right ventricular (RV) myocardium; fatty infiltration alone without fibrosis, which can occur as part of normal aging, is not sufficient. Localized or generalized dilation with myocardial thinning in regions of dilation can also be seen on MRI. Involvement of the posterolateral left ventricle is increasingly being recognized, leading some to prefer the term arrhythmic cardiomyopathy. Echocardiography is not sensitive for diagnosis and does not necessarily show the RV abnormalities, although RV dilation and dysfunction may become apparent echocardiographically as the disease progresses.
ARVC is a progressive condition, without evidence of the disease at birth despite presence of a mutation. RV enlargement tends to progress over time, although the rate differs among patients. Left ventricular involvement tends to become more prominent with time as well. β-blockers are recommended in all patients, as is limitation of high-intensity sports. Patients with documented VT should probably have implantable cardioverter-defibrillator (ICD) placement, with consideration of ICD for other patients based on risk assessment using a shared decision model.
Although the most common cause of sudden cardiac death among young athletes is hypertrophic cardiomyopathy on epidemiologic grounds, this patient’s ECG does not show the typical increased voltage, nor is there increased wall thickness on echocardiography (choice A is incorrect). Cardiac amyloidosis is an infiltrative disease that may have low voltage on ECG, which is not present in this tracing. Amyloidosis usually presents with heart failure, not ventricular tachycardia (choice D is incorrect). Brugada syndrome is a sodium channelopathy leading to an increased risk of sudden cardiac death. Brugada syndrome is diagnosed by coved ST-segment elevations in leads V1 and V2, not seen here (choice C is incorrect).234
A 34-year-old man collapses during a marathon. Bystander CPR is started, and an automated external defibrillator detects ventricular tachycardia (VT) and achieves cardioversion successfully. He has no known medical history, except for one previous syncopal episode during exercise. He has an uncle who died at 45 years in a single-car motor vehicle collision.
Echocardiography shows normal left ventricular size and performance with an ejection fraction of 55%. ECG is shown in Figure 1.
Which of the following is the most likely cause of the patient’s cardiac arrest?
Links to this note
-
- Contrast this with ARVC: epsilon wave on EKG is arrhythmogenic right ventricular cardiomyopathy
Footnotes
-
Cipriani A, Bauce B, De Lazzari M, et al. Arrhythmogenic right ventricular cardiomyopathy: characterization of left ventricular phenotype and differential diagnosis with dilated cardiomyopathy. J Am Heart Assoc. 2020;9(5):e014628. PubMed ↩
-
Towbin JA, McKenna WJ, Abrams DJ, et al. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy. Heart Rhythm. 2019;16(11):e301-e372. PubMed ↩