Brugada syndrome
- related: Cardiology and Hemodynamics, EKG basics
- tags: #literature #cardiology
Pathophysiology
- Na channel mutation
- triggered by stress or drugs
Brugada sign
-
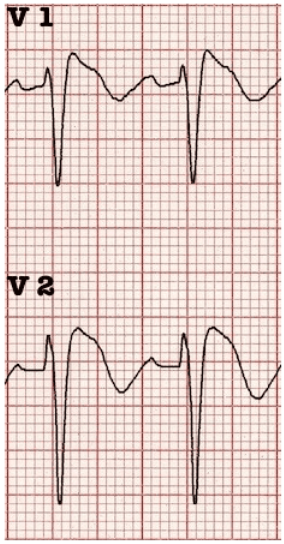
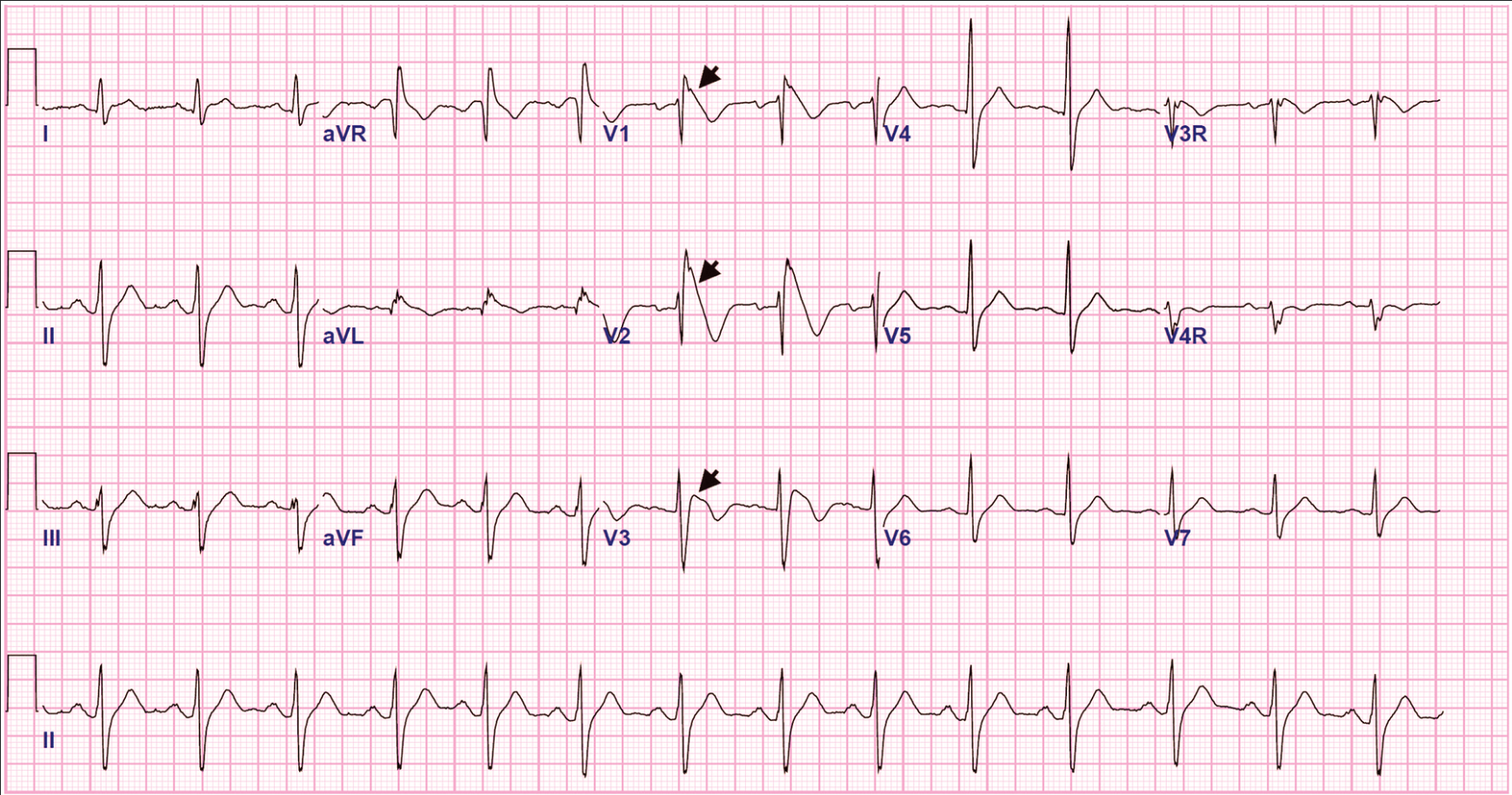
ST elevation in V1-V3 followed by negative T wave
-
Electrocardiogram demonstrating a type 1 Brugada pattern, ≥2 mm J-point elevation, ST-segment coving (concave or linear downsloping ST segment) (arrowheads), and T-wave inversions in leads V1 to V3.
-
Contrast this with ARVC: epsilon wave on EKG is arrhythmogenic right ventricular cardiomyopathy
Diagnosis
- must have Brugada sign + clinical criteria:
- Fhx sudden cardiac disease < 45 years old
- documented VF/VT
- Similar ECG in family members
- Inducible VT with electrical stimulation
- syncope
- nocturanal agonal respiration
Treatment
- ICD
Brugada syndrome is distinguished by right precordial ECG abnormalities, including ST-segment coving (concave or linear downsloping ST segment) in leads V1 to V3 with or without right bundle branch block, VF, and cardiac arrest (Figure 19). Brugada syndrome has an increased prevalence in men and persons of Asian descent. Arrhythmic events in patients with Brugada syndrome are more common at night during sleep. Abnormalities on ECG can be intermittent and may be elicited by fever or pharmacologic challenge with sodium channel blockade (such as with procainamide infusion). Patients with syncope or ventricular arrhythmia should undergo ICD implantation. Quinidine may be beneficial in patients with recurrent ventricular arrhythmias and/or ICD shocks.
Links to this note
-
CHEST fellow course 2024 Heme Onc Emergencies
- pseudo epsilon wave like in Brugada syndrome
-
epsilon wave on EKG is arrhythmogenic right ventricular cardiomyopathy
- Although the most common cause of sudden cardiac death among young athletes is hypertrophic cardiomyopathy on epidemiologic grounds, this patient’s ECG does not show the typical increased voltage, nor is there increased wall thickness on echocardiography (choice A is incorrect). Cardiac amyloidosis is an infiltrative disease that may have low voltage on ECG, which is not present in this tracing. Amyloidosis usually presents with heart failure, not ventricular tachycardia (choice D is incorrect). Brugada syndrome is a sodium channelopathy leading to an increased risk of sudden cardiac death. Brugada syndrome is diagnosed by coved ST-segment elevations in leads V1 and V2, not seen here (choice C is incorrect).[^2][^3][^4]