extrapulmonary tuberculosis
- related: Tuberculosis
- tags: #literature #pulmonology
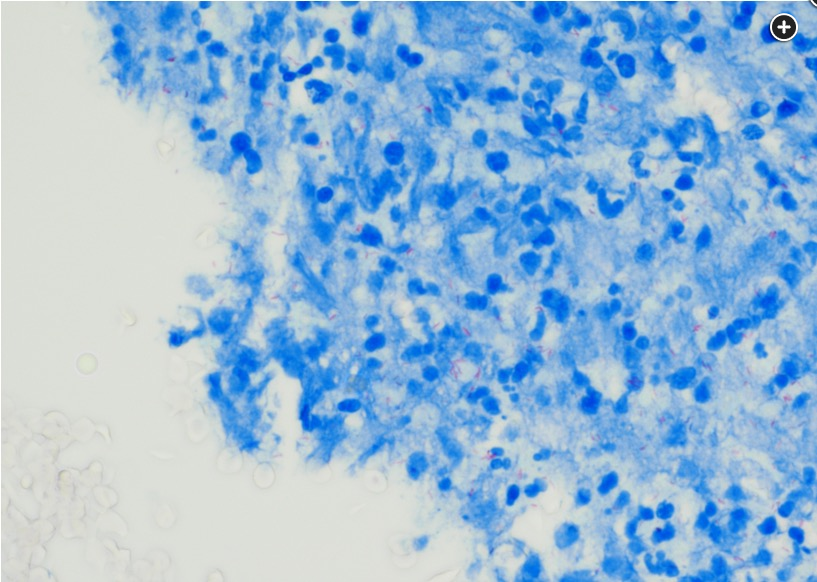
The patient has TB as acid-fast bacilli (AFB) are seen on BAL cytology (Figures 6 and 7). The omental biopsy was also positive for AFB (not shown). Many environmental, host, and microbial characteristics have been recognized as risk factors for dissemination of extrapulmonary tuberculosis (EPTB). A small subset (20%-40%) of patients with active TB infection present with either primary EPTB or EPTB with pulmonary involvement. (Most patients develop pulmonary TB.) Some studies suggest that the proportion of EPTB among all TB cases has been increasing in the United States mainly because of the increasing prevalence of HIV infection and other immunocompromised conditions. The most common sites of EPTB infection are lymph nodes, pleura, genitourinary system, GI tract, bones, and CNS. Genomic analysis suggests that dissemination of bacteria from lungs to extrapulmonary sites may occur as frequently as between lung sites.
EPTB is often unrecognized, and the diagnosis is often delayed owing to the atypical nature of the presentation. Risk factors for EPTB include age >45 years, HIV-positive status, end-stage renal disease, and excessive alcohol use within the past 12 months.
Treatment of EPTB is with first-line anti-TB drugs, and for some specific EPTB infection sites, adjuvant therapy with corticosteroids has also been used (choice A is correct). Rarely, surgical intervention is recommended when organ damage is occurring because of EPTB and when there is debilitation to the patient.
Because the bronchoscopy showed no bacterial organisms and another diagnosis has been established, there is no indication for bacterial pneumonia or fungal coverage (choices B and C are incorrect). Cytoreductive surgery to treat peritoneal tumor burden is also incorrect as the “peritoneal carcinomatosis” was in fact disseminated TB and there is no evidence of cancer. Disseminated TB is treated mainly medically and not surgically (choice D is incorrect).
With treatment, the patient had improved fever curve and lactic acidosis. She needed treatment regimen changes because of an increase in her liver function test results. She regained her appetite over several weeks, and her ascites dissipated.1