heparin induced thrombocytopenia and thrombosis HIT
- related: Hematology
- tags: #hemeonc
- HIT antibody has high false positive
- CABG patients have high false positive for HIT
- Use serotonin release assay to determine HIT in indeterminate HIT antibody test
- Stop anticoagulation in HIT when platelets have recovered
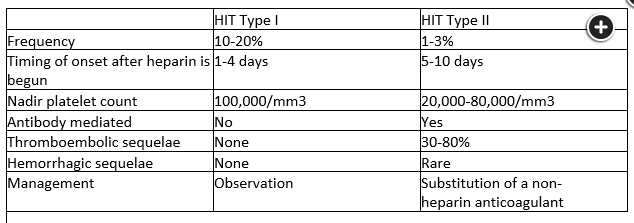
type 1 HITT
- within 2 days of initiating heparino
- transient, non pathologic
- Plt > 100k
- Do not stop heparin, plt will return to normal
type 2 HITT
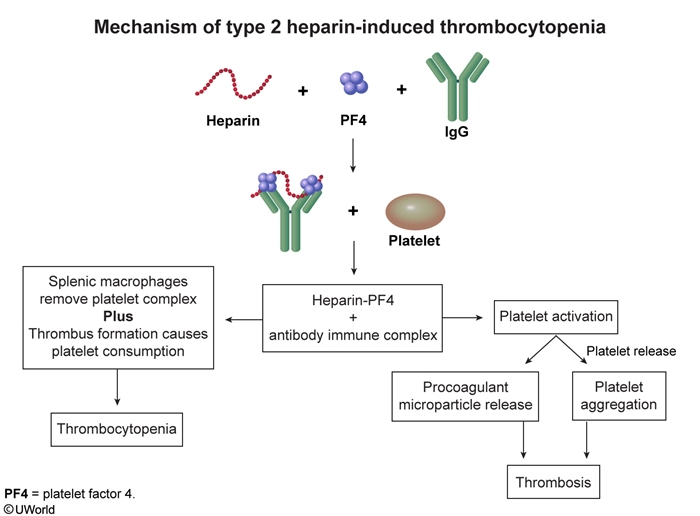
- antibody against PF4 => activates Plt => plt cascades => thrombosis and thrombocytopenia
- risks
- women
- most often unfractionated heparin
- CV surgery, ortho surgery, increased trauma severity
- more or longer heparin => more likely to get HITT
- patients with endothelial damage
- clotting is worse than bleeding
- arterial and venous clot
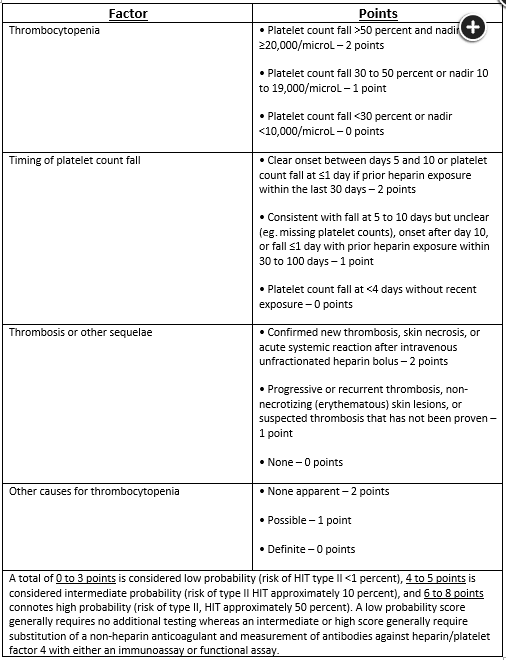
- Thrombocytopenia - platelets typically decline >30%-50%
- Timing - onset 5-10 days after heparin initiation or <1 day with prior, recent heparin exposure
- Thrombosis - new thrombosis, progressive thrombosis, or skin necrosis
- Alternative causes - no other sources for thrombocytopenia are present or likely
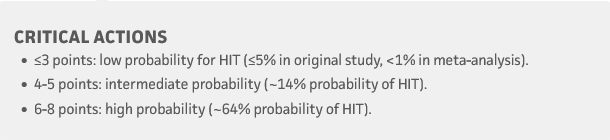
- interpret based on 4T score
- e.g. low 4T with positive test: 1% chance positive HITT
- Diagnosis is confirmed with serotonin release assays (preferred), heparin-induced platelet aggregation assays, or solid-phase immunoassays with ELISA for heparin-PF4 complexes.
- Stop argatroban: when Plt > 150k, then switch to DOAC or warfarin for minimum of 6 months. Initial treatment with warfarin is contraindicated as rapidly dropping protein C levels cause a prothrombotic state. Warfarin is usually started after the patient is treated with a non-heparin anticoagulant and recovers a platelet count to > 150,000/µL.
Heparin-induced thrombocytopenia (HIT) develops as a result of autoantibodies to platelet factor 4 complexed with heparin. Because the antibody activates platelets, arterial and venous thromboses can develop and can cause significant morbidity or death. When there is an intermediate or high probability of HIT based upon 4 Ts scoring, heparin should be stopped and replaced by a nonheparin factor Xa inhibitor or direct thrombin inhibitor while definitive serologic testing is performed. In addition to clinical examination for thrombosis and imaging of regions in which thrombosis is clinically suspected, 2018 guidelines recommend obtaining imaging studies to screen all individuals diagnosed with HIT for lower extremity deep vein thrombosis (choice D is correct). This recommendation is due to the high prevalence of asymptomatic deep venous thrombosis in the HIT population, plus the fact that the presence of deep venous thrombosis requires a period of anticoagulation of at least 3 months vs 4 weeks for HIT if thrombosis is not present.
While thrombosis involving intracranial arterial or venous structures may occur, they are rarely asymptomatic; therefore, cerebrovascular radiographic investigations are not indicated in asymptomatic individuals (choices A and B are incorrect). Likewise, the risk of cardiac thrombosis is not high in HIT, and echocardiography is not indicated for screening when HIT is diagnosed (choice C is incorrect).
Delayed onset HIT
Delayed-onset HIT - immune mediated due to high-titer antibodies against heparin-PF4 complexes in the absence of circulating heparin. Cases typically arise 5-19 days after heparin cessation; therefore, most patients present in the outpatient setting. Thrombocytopenia with or without life-threatening arterial or venous thrombosis are the norm.
[!NOTE] extensive DVT with thrombocytopenia after major surgery in clinic