icu lecture coagulopathy and bleeding
- related: ICU intensive care unit, massive transfusion protocol
- tags: #icu
Definition
- Coagulation: bleeding when you should; clotting when you should; no more and no less
- Coagulopathy: bleeding when you should not; clotting when you should not; more than less
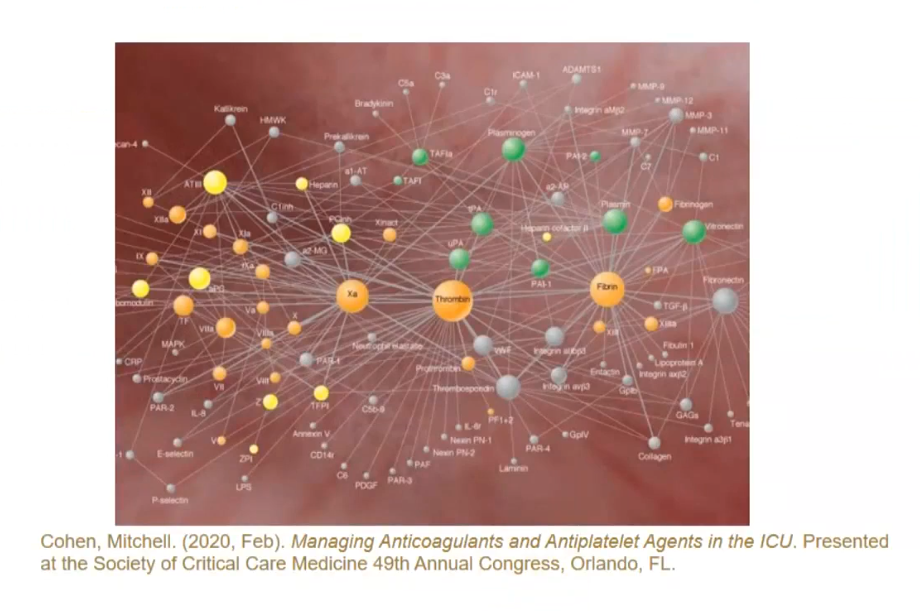
Intrinsic and extrinsic pathway do not exist in real life. Real life is more complex
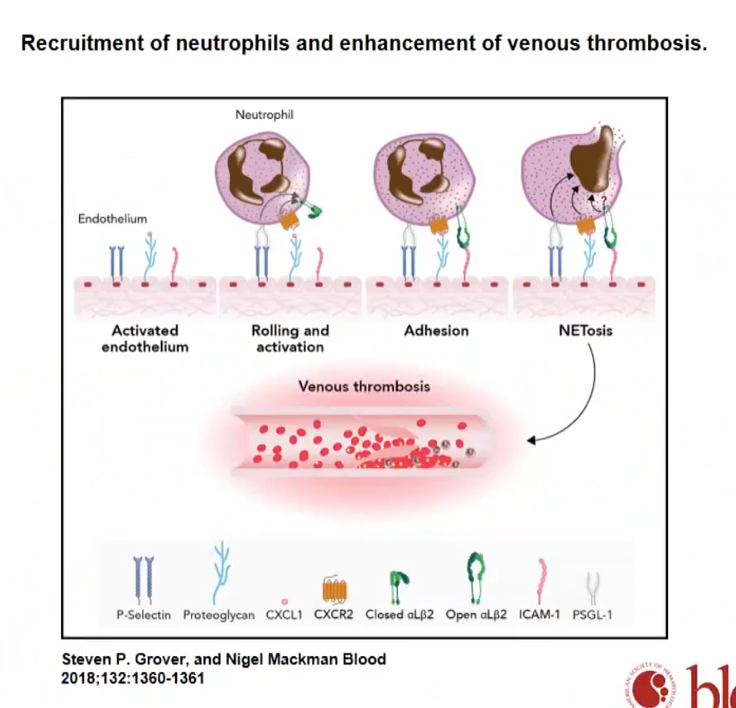
- immunothrombosis: activation of platelets and coagulation through PAMP and DAMP while using innate immune cells as inducers and regulators
- you have to have functional immune system to have coagulation
- leukocytes also line endothelium to maintain laminar flow. Lack of it can cause thrombosis and bleeding
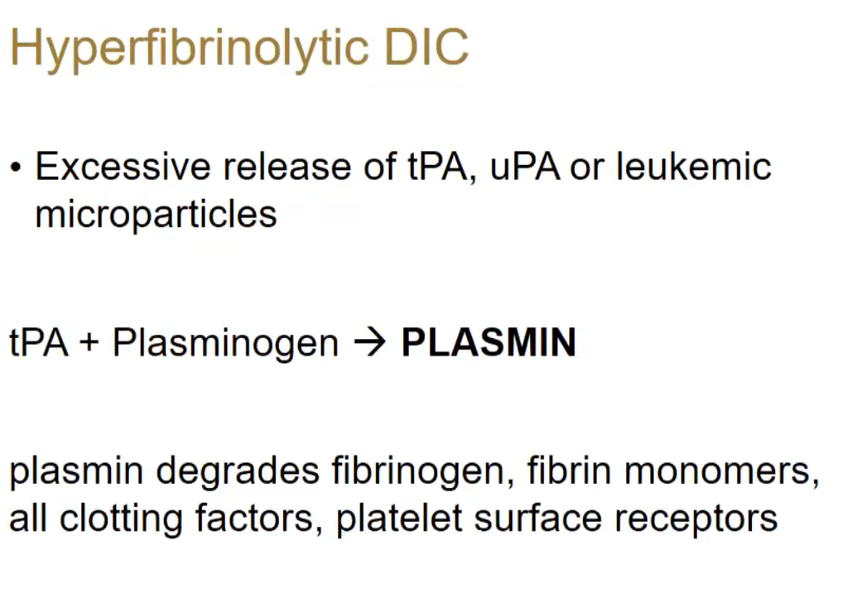
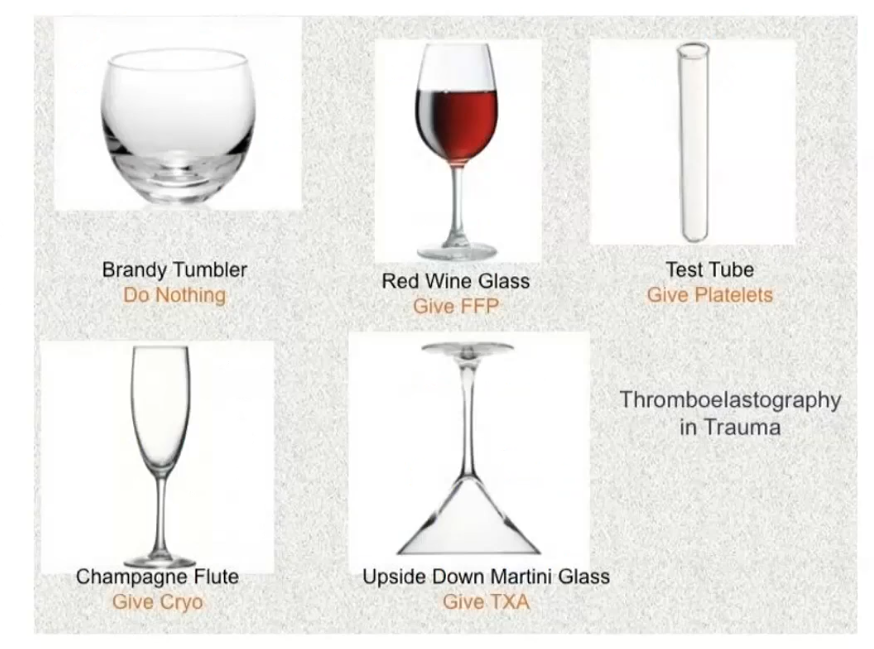
txa
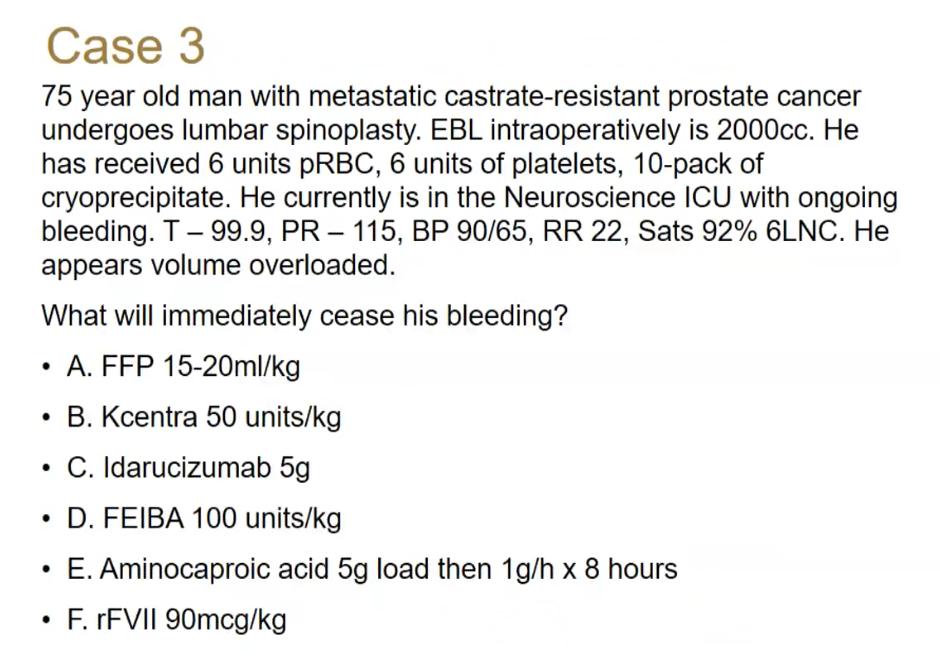
- TXA: aminocaproic acid. Changes blinding site of plasmin
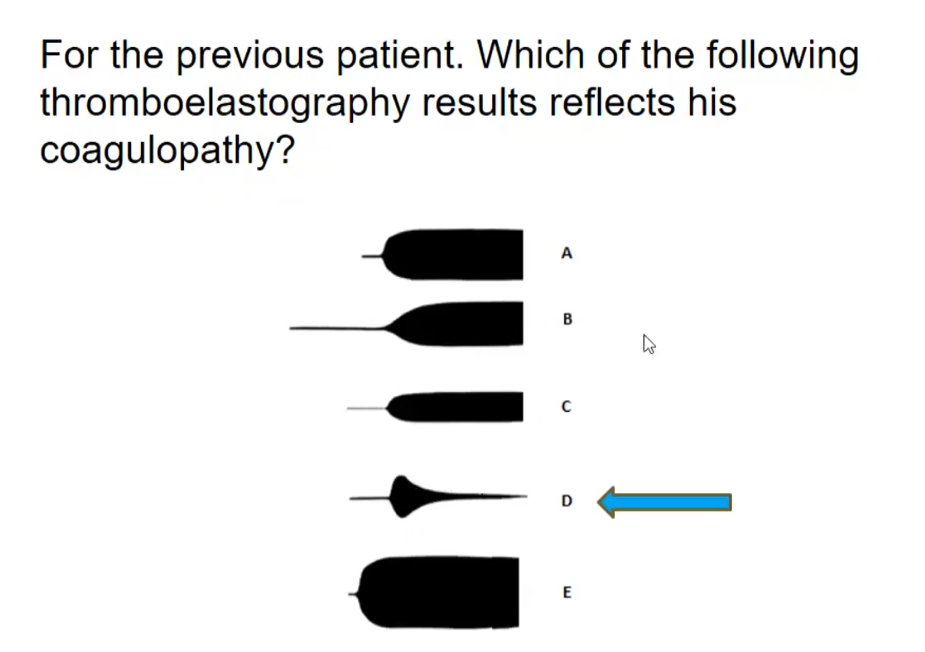
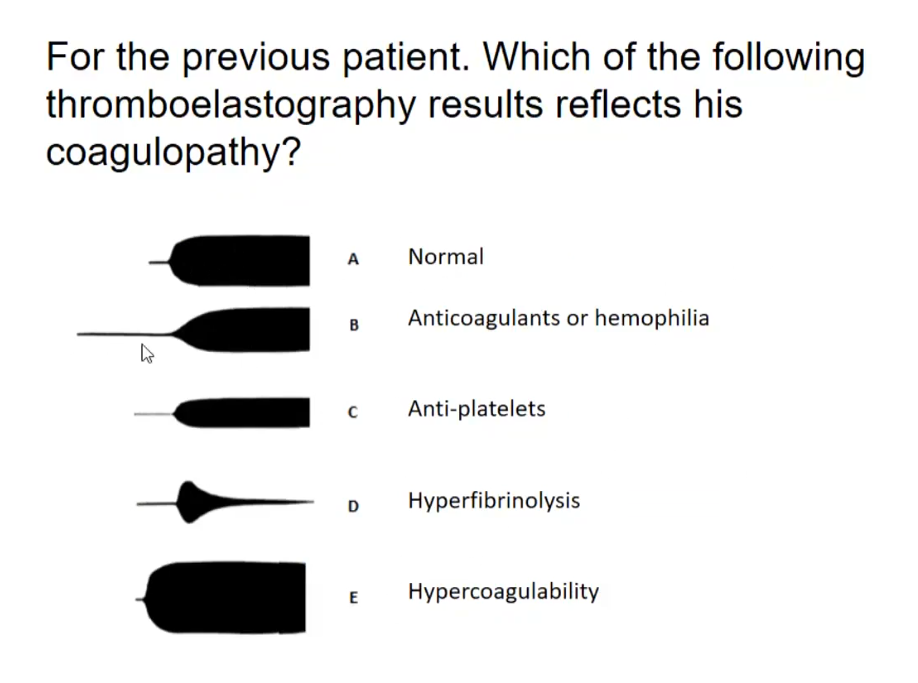
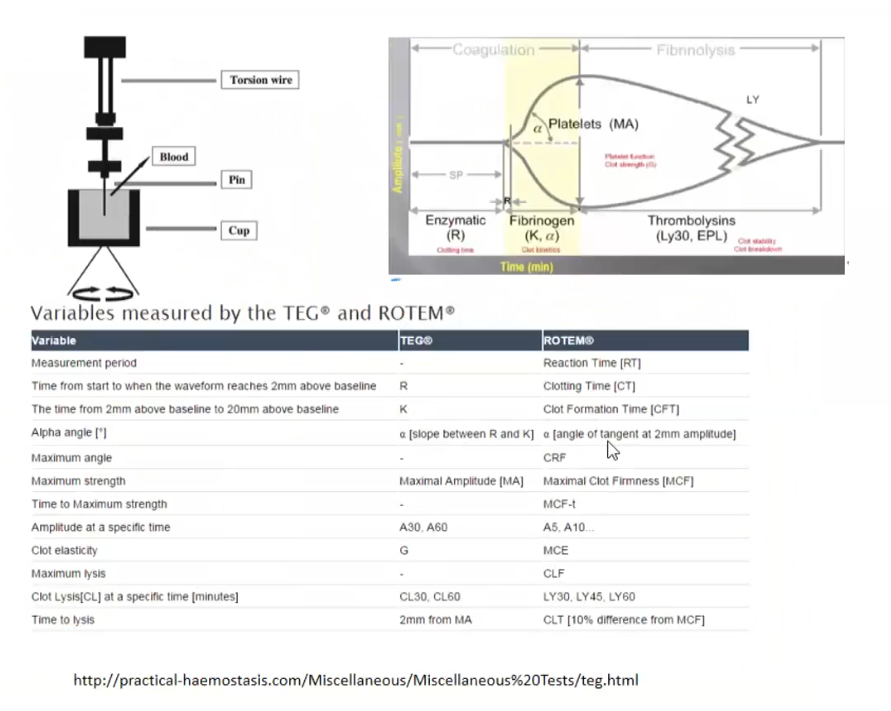
- TEG tracing
TTP
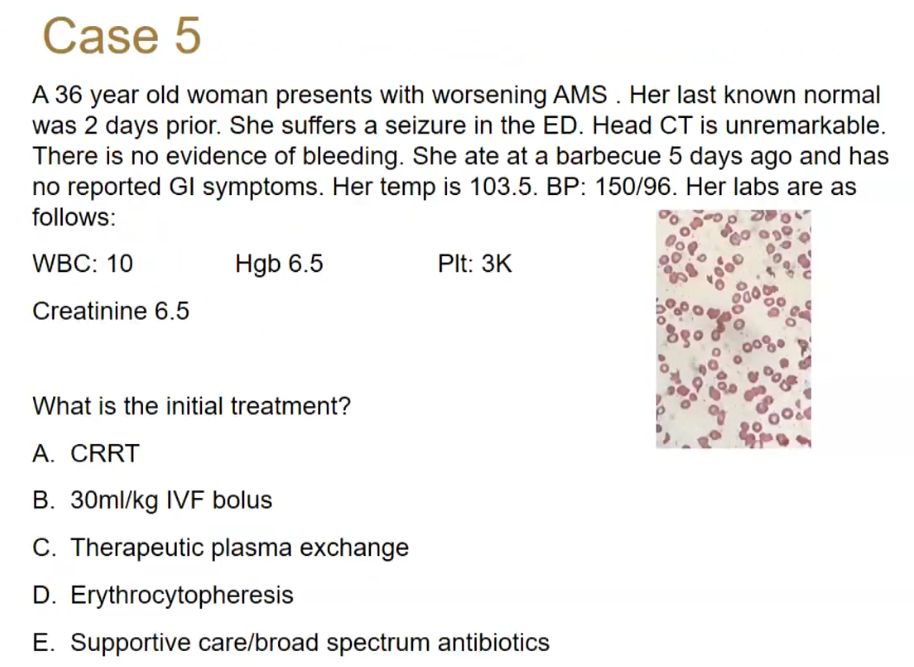
- TTP: therapeutic plasma exchange
- plasma exchange: replace plasma and ADAMTS13
- plasmaphresis: just filters plasma
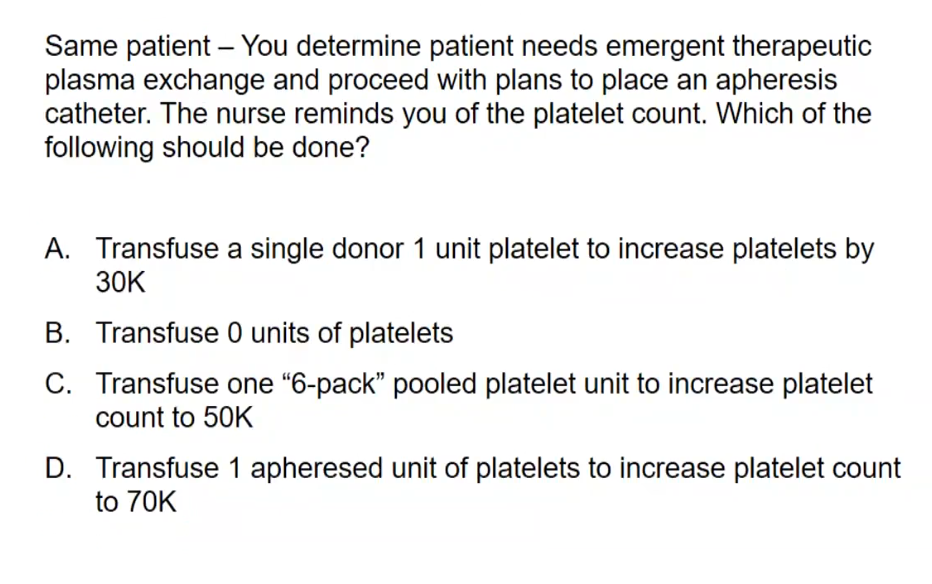
- don’t tranfuse
- TTP patients tend to not bleed. Few thousand plts left seem to be hyperactive. If pt ooze a lot when catheter in, probably not TTP. If not bleeding when place catheter, probably not TTP.
- not based on trials
- transfuse during procedure
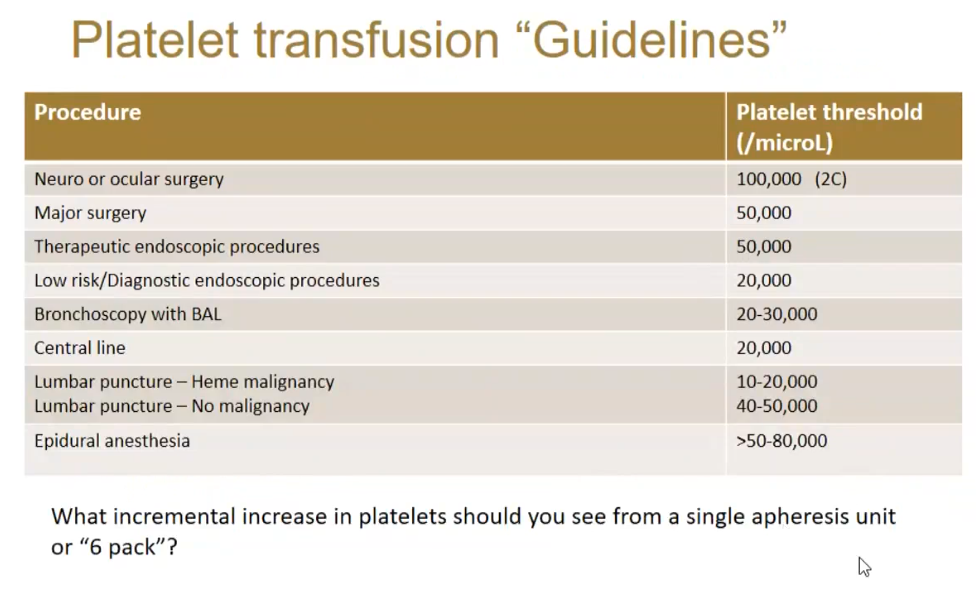
- plt increase by 30k (15-45) for single unit, peaks in 10 min - 1 hour
CTS induced
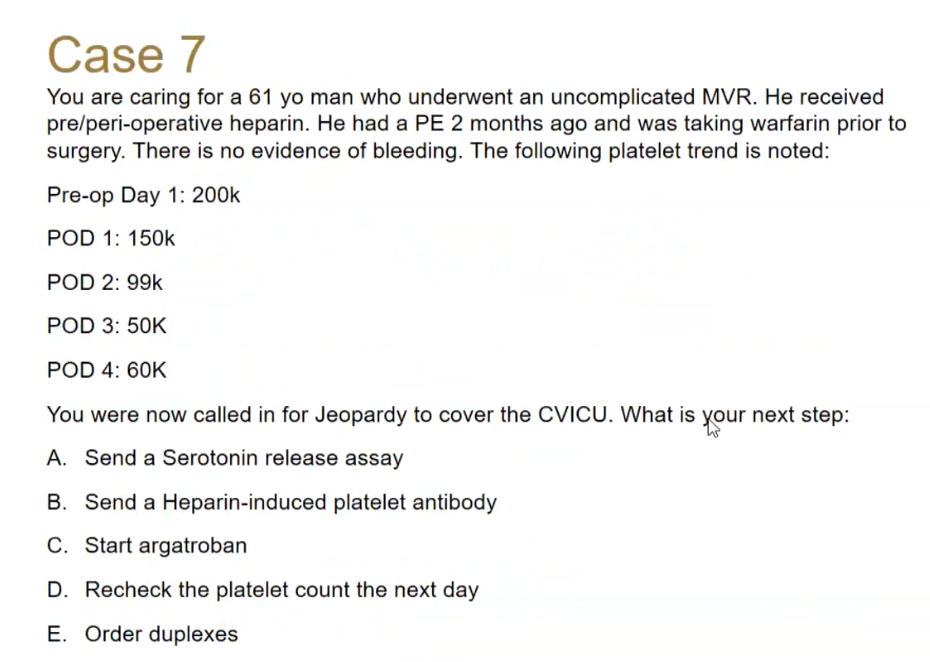
- recheck plt
- heparin induced antibodies post CT surgery
HIT
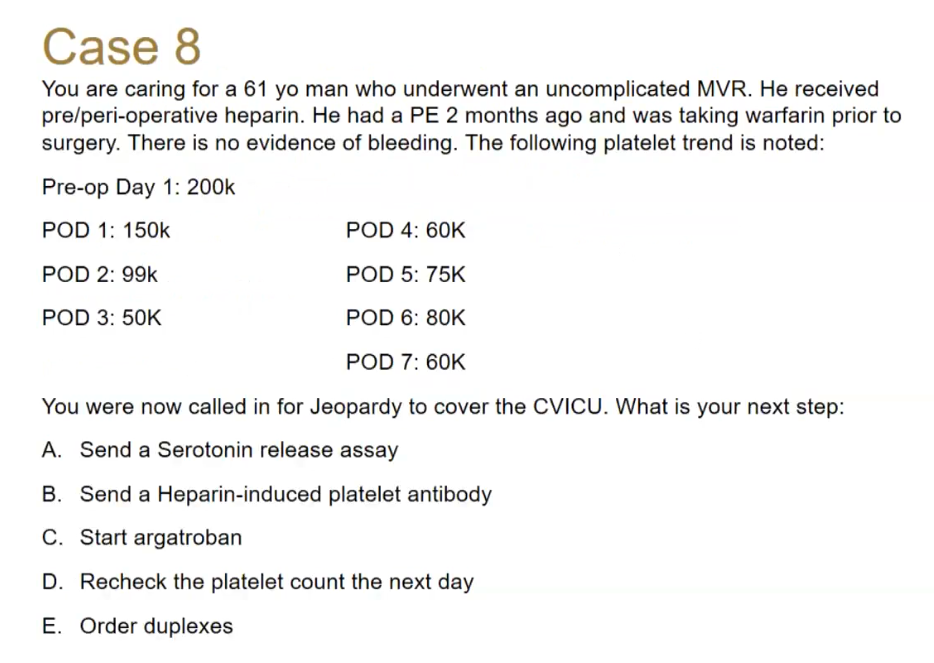
- work up for HIT with A-E
- duplex in all extremities
- calculate 4T
- nadir, go back up and then drop again instead of continue to recover
- other causes: CRRT, cancer
Heyde
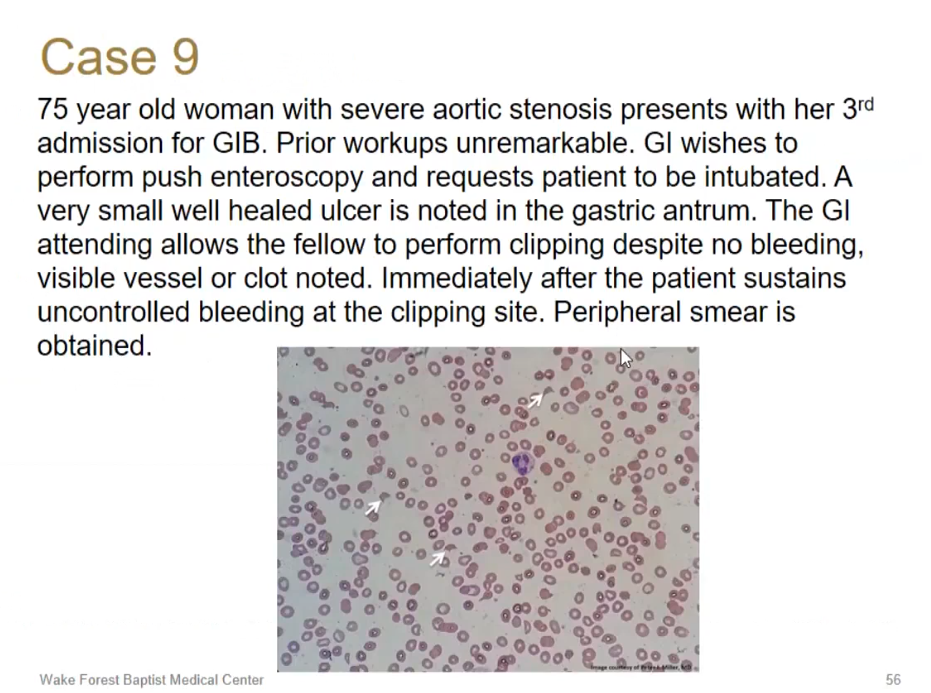
- Heyde’s syndrome
- angiodysplasia and cleavage of vW multimers
surgical
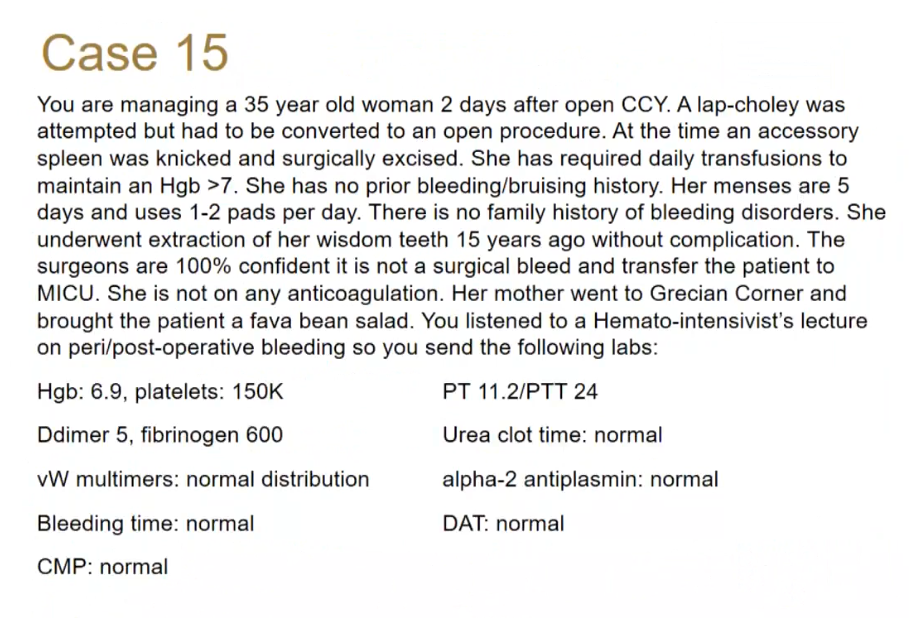
- prolene deficiency: surgical problems. Call surgery