look for rebleed potential in SAH patients
- related: Neurology
- tags: #icu #literature
Subarachnoid hemorrhage (SAH) is a common neurological entity in the ICU. The diagnosis of SAH is classically made by a patient history of acute-onset severe headache (“worst headache of my life”) and neck stiffness plus a noncontrast CT scan showing evidence of blood in the subarachnoid space. Lumbar puncture (LP) is reserved for patients who present with a convincing symptom complex for SAH but no evidence of blood on CT scans.
In this patient, the CT scan shows bright signal in the cerebrospinal fluid spaces around the brain parenchyma (the subarachnoid space), which represents blood outside of blood vessels (Figure 2, white arrows).
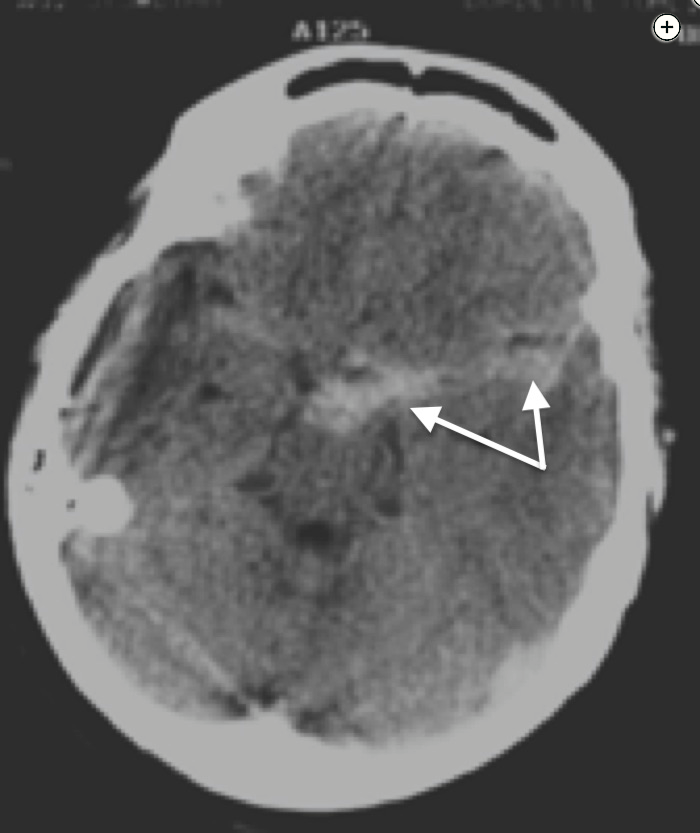
Noncontrast CT scan of the head showing subarachnoid hemorrhage (arrows).
In patients with diagnosed SAH, the most important early consideration is to identify whether a vascular abnormality exists that could rebleed. Rebleeding in SAH is the most debilitating secondary injury. The initial workup focuses on exploring the presence of an intracranial aneurysm by CT arteriography or digital subtraction angiography. In patients in whom an aneurysm is not found, a second delayed cerebral angiogram is often done, as there is a theoretical risk that vascular dye studies can miss an aneurysm in the acute phase because thrombosis after hemorrhage can exclude dye from the abnormality. The practice of repeating conventional digital subtraction angiography after a period of time (typically 5-14 days) to make sure that a recanalized aneurysm does not exist has been called into question by two case series that showed that patients with negative initial angiograms have little risk of having a residual aneurysm identified by a subsequent angiogram or by recurrence of SAH.
Other less common causes of SAH can have significant sequelae. Particularly, cerebral vasculitis and arteriovenous malformations (AVMs) can cause SAH. Cerebral vasculitis can represent either isolated CNS disease (cerebral angiitis) or cerebral involvement of systemic vasculitis (such as polyarteritis or temporal arteritis). Rebleeding per se is not as important a consequence, but undertreatment due to late identification can lead to significant morbidity from stroke or intraparenchymal hemorrhage. Both MRI of the brain and cerebral digital subtraction angiography are appropriate tests to evaluate for cerebral vasculitis.
Although cerebral angiography is sufficient to rule out cerebral AVMs, SAH caused by spinal AVMs is increasingly reported. These are often missed on conventional digital subtraction angiography unless selective spinal artery interrogation is performed (which is reserved for patients with high risk of spinal AVM because the test is time-consuming and technically challenging). MRI of the spine is an appropriate imaging technique to diagnose spinal AVMs (choice B is correct). Spinal AVMs can lead to neurological disability in two ways: bleeding causing damage to the spinal cord or brainstem or development of spinal cord ischemia on the basis of venous hypertension from the arterialization of the spinal draining veins, which leads to spinal infarction and paralysis.
Because this patient has evidence of blood on the initial CT scan, there is no role for LP, particularly 7 days after the initial symptoms (choice C is incorrect). The role for LP for the diagnosis of SAH is unclear. Initial studies that showed the benefit of LP were conducted in the era of early generation CT scanning where false-negative results were common. With newer, higher-resolution CT scanners, the false-negative rate is unclear and likely very low. One possible workflow is to stratify patients with suggestive history of SAH and those with less typical symptoms. For CT-negative patients with suggestive history, CT angiography or conventional cerebral arteriography to identify aneurysms is recommended (followed by spine MRI if no aneurysm is identified). For patients with less suggestive history, reassessment for other etiologies of the headache is warranted.
As described, two angiograms are sufficient to identify nonvisualized cerebral aneurysms, so a third angiogram is not recommended (choice A is incorrect). MRI of the brain is as sensitive a test for SAH as conventional CT scanning but, in the acute setting, offers no advantage over CT scanning of the head and is more expensive and often less available (choice D is incorrect). MRI may be more useful than CT scanning to diagnose nonaneurysmal causes of SAH such as vasculitis but, because this patient has already had two angiograms, vasculitis should no longer be a consideration.
Treatment of spinal AVMs is best accomplished by a combination of endovascular embolization and surgical resection. The choice of how to address these malformations has a great deal to do with the anatomical characteristics of the AVM and assessment of interventional risk.12345
A 44-year-old man presents with acute onset of headache and neck stiffness. The CT scan is shown (Figure 1). A CT angiogram and a digital subtraction angiogram of the brain show no evidence of a cerebral aneurysm. The ICU and hospital course are uneventful. At day 7, a repeat cerebral angiogram shows no evidence of aneurysm. What is the next appropriate step in the evaluation?
Links to this note
Footnotes
-
Bashir A, Mikkelsen R, Sørensen L, et al. Non-aneurysmal subarachnoid hemorrhage: when is a second angiography indicated? Neuroradiol J. 2018;31(3):244-252. PubMed ↩
-
Carpenter CR, Hussain AM, Ward MJ, et al. Spontaneous subarachnoid hemorrhage: a systematic review and meta-analysis describing the diagnostic accuracy of history, physical examination, imaging, and lumbar puncture with an exploration of test thresholds. Acad Emerg Med. 2016;23(9):963-1003. PubMed ↩
-
Cerejo R, John S, Grabowski M, et al. Thoracolumbar arteriovenous malformations presenting with intracranial subarachnoid hemorrhage: case series and review of literature. World Neurosurg. 2016;88:182-187. PubMed ↩
-
van Beijnum J, Straver DC, Rinkel GJ, et al. Spinal arteriovenous shunts presenting as intracranial subarachnoid haemorrhage. J Neurol. 2007;254(8):1044-1051. PubMed ↩