Lung nodules
- related: Pulmonary Diseases, lung mass and cancer
- tags: #pulmonology #literature
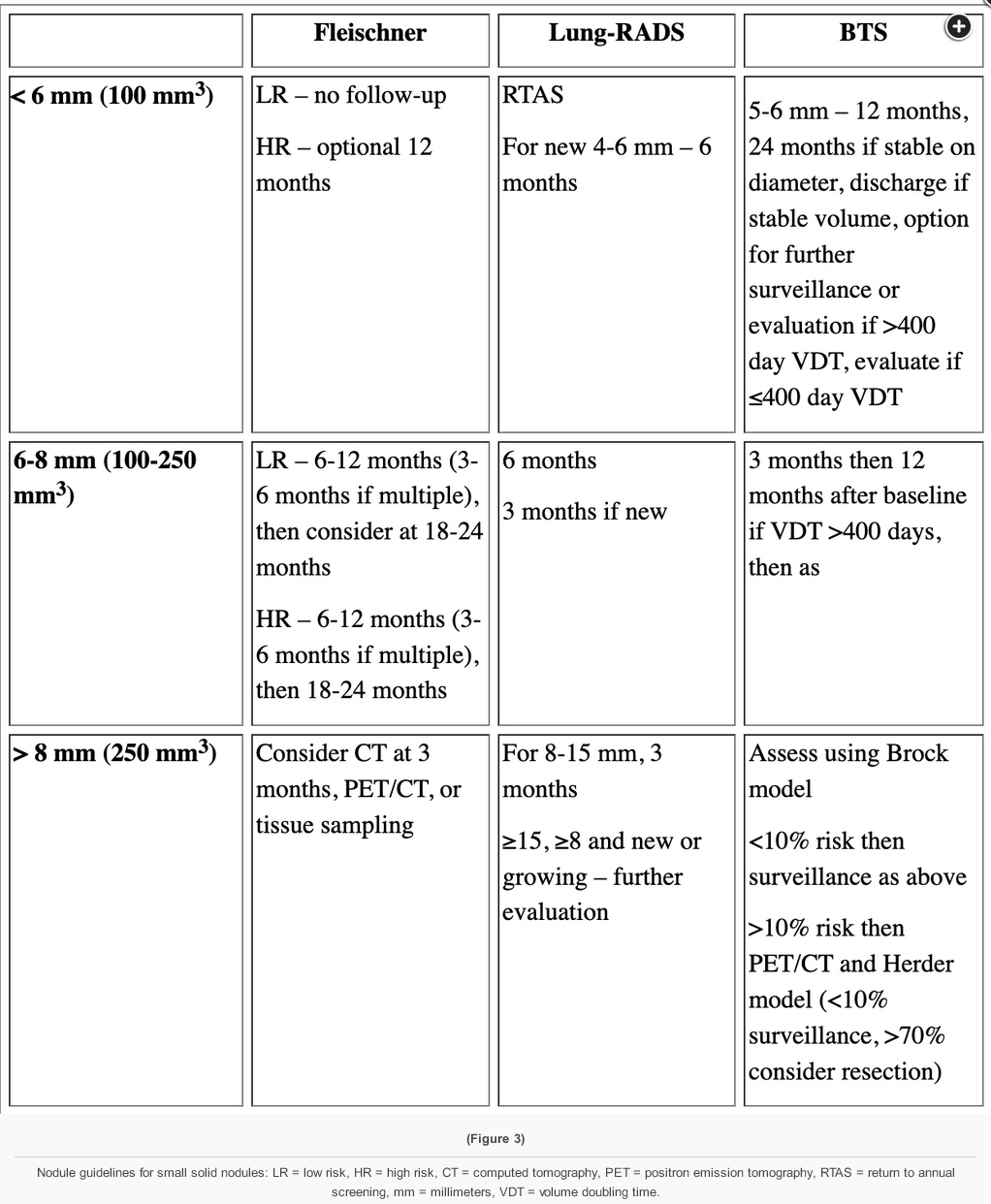
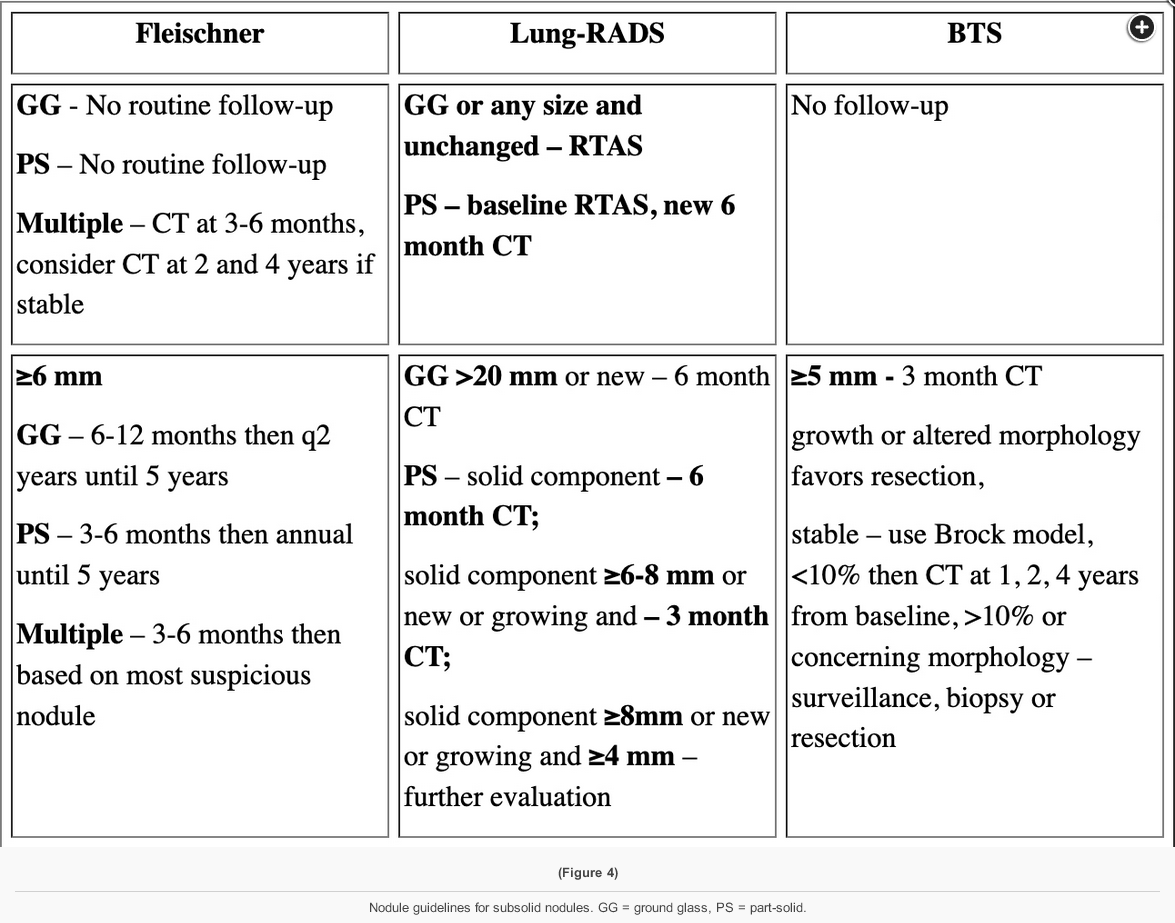
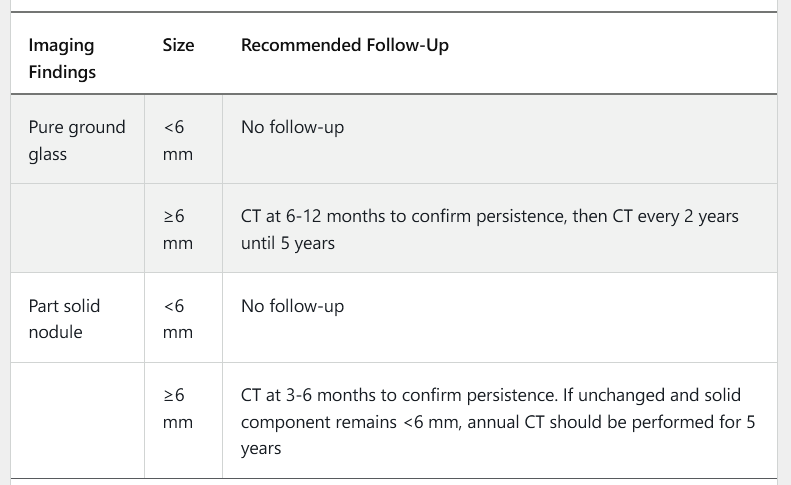
Solid nodules and subsolid nodules (pure ground glass and part-solid nodules) have different rates of malignancy and different growth rates when malignant, thus the management recommendations differ for these two categories of lung nodules. Subsolid nodules that are malignant represent a more indolent type of lung cancer with slower growth. Therefore, follow-up intervals are spaced more widely and the duration of follow-up is increased. Recommendations for evaluation of a 6 mm solid nodule and a 6 mm pure ground glass nodule include the same initial surveillance interval (6-12 months) but different additional surveillance intervals (12 months later for the solid nodule and 2 years later for the ground glass nodule)1
- features:
- Rounded opacity
- ≤3 cm in diameter (>3 cm is considered a “mass” and malignant until proven not)
- Surrounded by pulmonary parenchyma
- No associated lymph node enlargement, not associated with atelectasis, hilar enlargement, pleural effusion
Solid Nodule > 8 mm
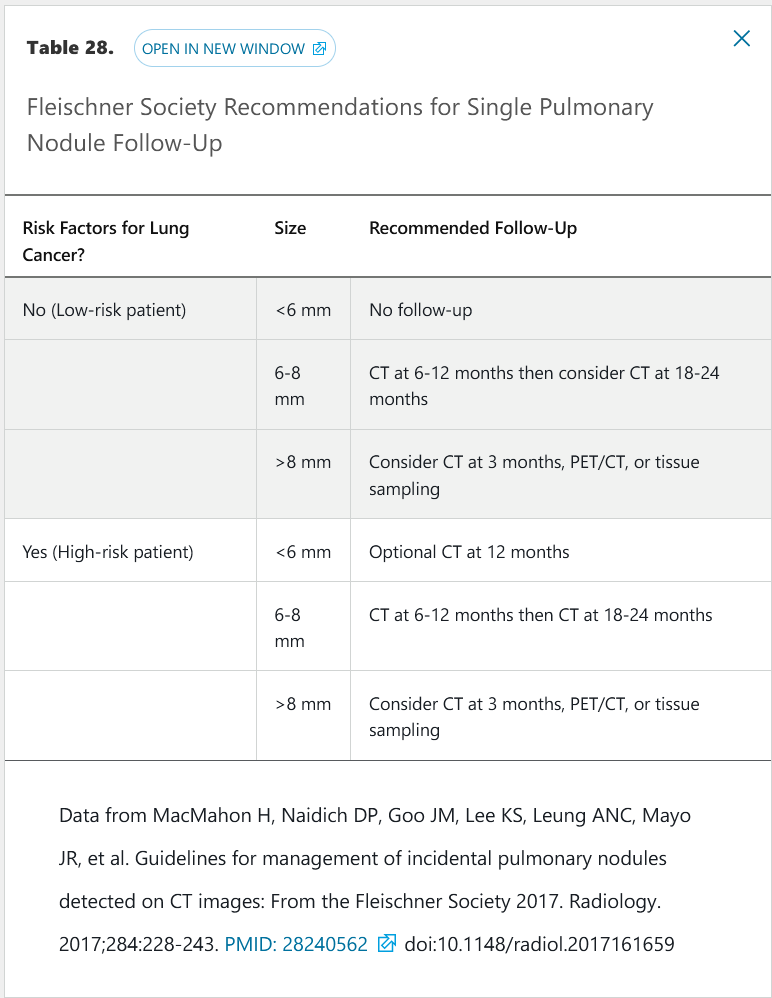
- low/moderate probability: PET scan
- PET neg: continued surveillance
- PET positive: staging, resection/chemo/radiation
- high probability: PET, then resection/chemo/radiation
Solid Nodule =< 8mm
- usually serial CT scans
Subsolid Nodule
- focal rounded opacity either pure ground glass (focal density with underlying lung architecture) or solid component but has >50% ground glass
- usually premalignant disease, such as adenocarcinoma in situ
- can be slow growing
- growth rate 400-800 days
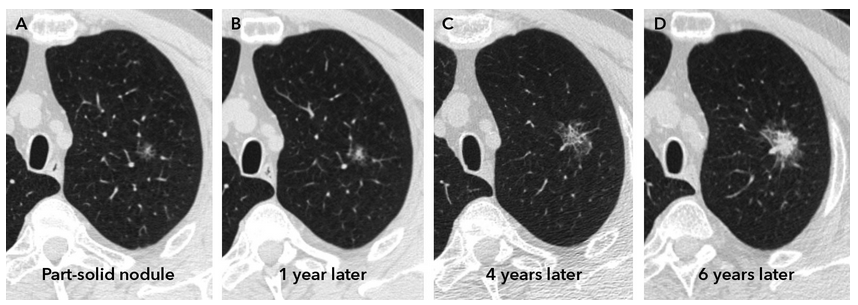
- evolution of part solid nodule from adenocarcinoma in situ to invasive adenocarcinoma
management
- compare prior xray or CT
- if stable appearance/size 2-3 years, no further workup
- if change in appearance, obtain CT
- if no prior CT/xray, obtain CT to identify other lesions
- if >0.8 cm, further management (biopsy) and surveillance
- PET can be used if tissue diagnosis unclear
- benign characters:
- round appearance
- ground glass
- < 0.6 cm
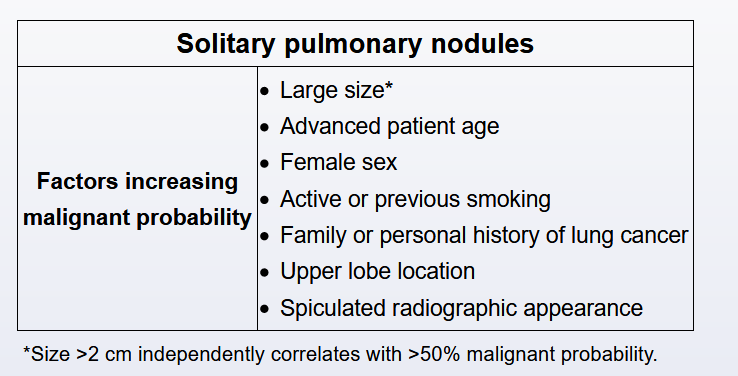
- malignant characters:
- partially solid (heterogenous)
- spiculated appearance
- >0.8 cm upper lobe location
Certain patterns of calcification within the pulmonary nodule are strongly suggestive of benign lesions, including popcorn, concentric or laminated, central, and diffuse homogeneous calcifications. Popcorn calcification is characteristically seen on radiographic imaging in patients with pulmonary hamartoma. Eccentric calcification (area of asymmetric calcification), as well as reticular or punctate calcification, should raise suspicion for malignancy.
8/2021 notes
- lung nodule spread: hilum to mediastinum to opposite hilum
- make sure hilum/mediastinum not involved
Type
- ground glass: mostly infection/inflammation
- adenocarcinoma in situ, grow more slowly
- PET scan not helpful
- follow 2 year interval, watch for very long time
- adenocarcinoma in situ, grow more slowly
- Solid: most common
- Subsolid: most likely cancer
- Typing: acute, subacute, chronic
Size
- < 3 cm
- subsolid > 5 mm
DDx
- cancer:
- breast: 50/50 primary breast vs lung
- ENT: mostly lung primary
- sarcoma: mostly lung mets
- Infection: MRSA, fungal, aspergillosis (more ground glass from hemorrhage around nodule, halo effect)
- rheumatolgy: RA, sarcoid, Wegener
- benign
Management
- high probability: PET: 30% false positive
- biopsy: EBUS vs TTFNA (25% pneumothorax, 5% chest tube)
- surgery resection
- low probability: CT surveillaince 3 month to 1 year
- intermediate: 10-60%, CT, PET, biopsy
Patients risk factor
- age is biggest risk factor
- smoking
- cancer hx
- COPD
- FHx can be important
- work exposure
- asbestosis: 20-30 years latency, pleural plaque
- BAPE benign asbestos related pleural effusion: effusion, eosinophil predominant, unilateral effusion
- construction working
- ship building
- brake pads
- radon
Nodule risk factors
- size
- <6mm, 6-8mm, >8mm
- border/edge
- smooth, well circumscribed
- lobulated: uneven growth
- spiculated
- corona radiata
- calcification
- benign: popcorn, laminar, granulomatous, central fat
- malignant: stippled, ecentric, subsolid, ground glass
- location: higher probability in apex
Scoring
- solidary pulmonary nodule malignancy (SPN) risk score
- mayo clinic: incidental solid nodule
- Brock: nodules found on lung screen
- Fleischner risk
Others
aVS: .lungcancerscreen and .lungcancerscreenAVS
Links to this note
-
CT scan for robotic bronchosocopy
- related: Lung nodules
-
- related: Lung nodules