marijuana use can induce bulla formation
- related: Pulmonology
- tags: #literature #pulmonology
Source
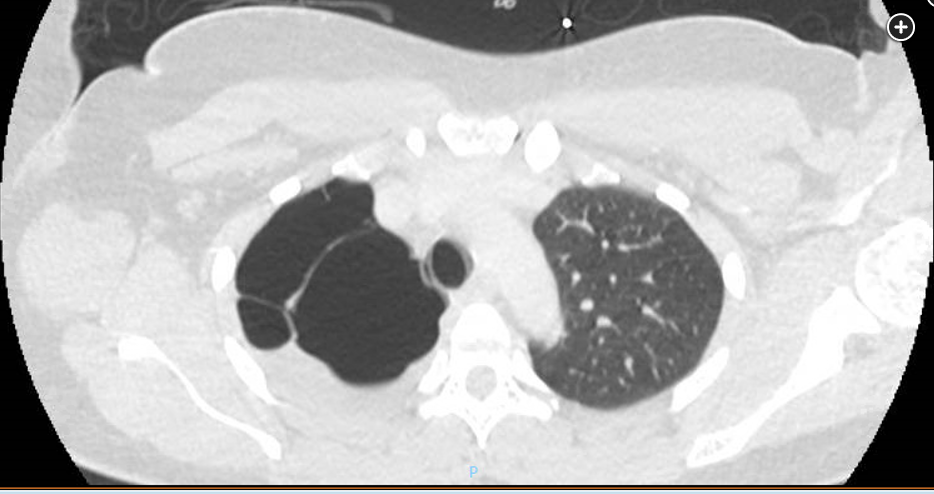
The most likely etiology of this patient’s giant bullae is marijuana use. Use of marijuana is associated with impaired short-term memory, impaired motor coordination, altered judgment, paranoia, psychosis, altered brain development, and symptoms of chronic bronchitis. Pneumomediastinum, pneumothorax, and subcutaneous emphysema have been reported with deep inhalation of marijuana involving breath holding. Case series have shown severe bullous lung disease in the upper lobes of the lungs among marijuana smokers. The mechanism for bullae formation in marijuana users may be the combination of the direct toxic components in marijuana and the prolonged breath holding that can generate high inspiratory pressure leading to barotrauma. Inflammatory cells in marijuana smokers may cause pulmonary toxicity that may cause loss of lung elastic recoil leading to bulla formation.
In most cases, bullous lung disease is caused by prolonged exposure to smoke. This may be from combustion of tobacco or other biomass fuels used for heating or cooking, such as wood, coal, peat, and kerosene. Cigarette smoke accounts for the vast majority of disease, but smoke from burning of biomass fuels in poorly ventilated stoves or open fires used for cooking and heating is an important secondary cause worldwide.
Although exposure to organic or inorganic dusts, industrial chemicals, and outdoor air pollution may also play a role, the evidence linking these exposures to bullous lung disease is not nearly as strong as that for cigarette and biomass fuel smoke.
In bullous emphysema, bullae are created as areas of severe emphysema coalesce due to progressive loss of alveolar attachments. In general, the epidemiology of bullous lung disease closely follows that of COPD. Affected individuals tend to be older (usually >45) and have significant exposure to tobacco smoke (usually at least 10 pack-years).
Genetic factors may also contribute to development of bullous lung disease, such as alpha-1 antitrypsin deficiency. This increases susceptibility to smoke-induced bullous emphysema and, much less commonly, may cause significant emphysema in the absence of smoking. Alpha-1 antitrypsin deficiency usually causes basilar predominant emphysema with a relatively young age of onset (often younger than 40-45), but it can also cause apical-predominant or homogeneous emphysema in older individuals.
Inherited connective tissue disorders, such as Marfan and Ehlers-Danlos syndrome, have been linked to increased risk of bullous lung disease and pneumothorax. However, these disorders more commonly cause small apical blebs rather than large intraparenchymal bullae.
Cystic lung diseases (eg, lymphangioleiomyomatosis, pulmonary Langerhans cell histiocytosis) are usually associated with smaller cysts that have a perceptible wall; this patient’s large bullae do not have a perceptible wall (choices A and B are incorrect). Patients with Marfan syndrome can develop apical bullae, but these generally do not meet criteria for giant bullae, and her body habitus was not consistent with Marfan syndrome (choice C is incorrect). Other genetic diseases, such as neurofibromatosis type 1 and Birt-Hogg-Dube, have been associated with giant bullae in case reports. These diseases typically cause cystic lung disease, and as such CT chest scan shows giant bullae along with numerous smaller cysts throughout the lungs, not just the large apical cystic disease.1