Mounier-Kuhn Syndrome or tracobronchomegaly
- related: Pulmonology
- tags: #literature #pulmonology
- etiology: atrophy of elastic fibers in trachea and major airways
- patient: usually younger, recurrent pneumonia
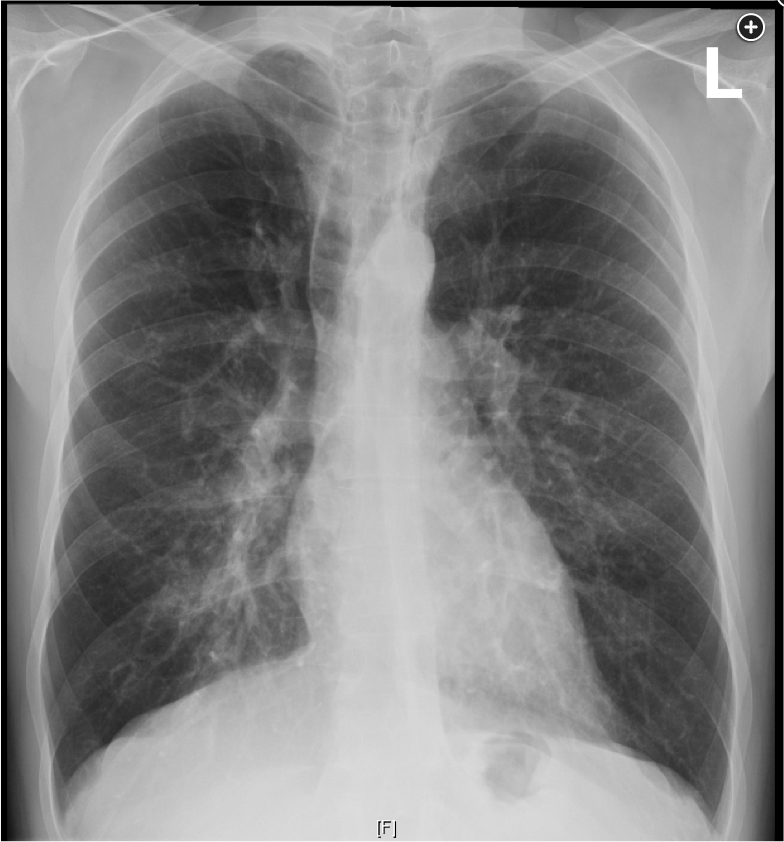
- CXR: dilated trachea
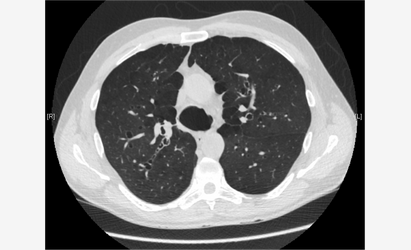
- CT: dilated trachea and maybe normal peripheral airways. Can sometimes have both emphysema and bronchiectasis
- CT: airway dilated on inspiration and narrow on expiration
Source
This patient has Mounier-Kuhn Syndrome (tracheobronchomegaly), an uncommon condition characterized by dilatation of the trachea and major bronchi, with normal-diameter peripheral airways (choice A is correct). The dilated trachea and major bronchi are associated with an inefficient cough and impaired mucociliary clearance, leading to recurrent respiratory tract infections and subsequent bronchiectasis. Airway diverticula may develop and retain secretions. Diagnosis is made based on findings on chest radiographs when the transverse diameter of the trachea is >3.0 cm or, as a general rule, when the lower trachea is wider than the vertebrae at the same level. On chest CT scan, a tracheal diameter >3 cm measured 2 cm above the aortic arch is used.

The pathophysiology of Mounier-Kuhn syndrome relates to atrophy or absence of elastic fibers in the tracheal wall, often with loss or thinning of airway smooth muscle. Etiology is unclear but may be due to congenital defects of elastic tissue in some patients. Airways markedly dilate on inspiration and narrow on expiration. Patients with Ehlers-Danlos syndrome can have marked dilatation of the trachea due to altered synthesis and processing of collagen. This inherited condition, however, is characterized by joint hypermobility and skin hyperextensibility, which are not noted in this patient (choice B is incorrect).
Mounier-Kuhn syndrome is one of the few conditions in which both bronchiectasis and emphysema can occur concomitantly (in the absence of smoking) owing to abnormal airway dynamics, retained secretions, and possibly a ball-valve mechanism. Transient obstruction may lead to infection and worsening bronchiectasis. α-1 antitrypsin (AAT) deficiency can also lead to this combination (although many patients are smokers). The diagnosis of AAT deficiency is made by demonstrating a serum AAT level <57 mg/dL (11 µmol/L) in the setting of specific genotypes. A level >80 mg/dL (15 µmol/L) is unlikely to cause disease (choice C is incorrect). The emphysematous changes noted in this patient likely reflect Mounier-Kuhn disease and his significant smoking history, despite his young age.
Typically, symptoms are nonspecific and are secondary to lower respiratory infections, bronchiectasis, airway narrowing, and/or fibrosis. Many patients do not show symptoms until the third decade of life (which may suggest an acquired etiology). Management centers on chest physiotherapy and antibiotics during exacerbations. Surgical options are limited because of the diffuse and central nature of the disease, though one limited series reported improvement in symptoms by using stenting or surgical tracheobronchoplasty. Mucinous stent impaction was cited as a frequent complication.
Primary ciliary dyskinesia leads to poor mucociliary clearance, and recurrent sinopulmonary infections and subsequent bronchiectasis, but the trachea and main bronchi are not enlarged (choice D is incorrect).1