osler weber rendu is associated with pulmonary AVM
- related: Pulmonary Diseases
- tags: #literature #pulmonology
The patient has HHT, formerly known as Osler-Weber-Rendu, on the basis of positive genetic test results. HHT is an autosomal dominant disease associated with vascular malformations that may occur in numerous organ systems. The vascular lesions include telangiectasias, which are small dilated blood vessels, and arteriovenous malformations (AVMs), which are vascular structures with direct communication between the arteries and veins. Telangiectasias occur on the skin and mucous membranes and result in epistaxis and GI bleeding with consequent anemia. AVMs most commonly occur in the lung, liver, and brain. Pulmonary AVMs may result in embolization of clot or bacteria from right-to-left shunt to the cerebral circulation, with cerebral vascular accidents and cerebral abscesses as a result.
HHT occurs in 1 in 5,000 individuals, but only 10% of affected individuals have received this diagnosis. The diagnosis is based on the Curaçao Diagnostic Criteria or genetic testing. In patients with HHT diagnosed, 80% will have a mutation in the ENG (HHT type 1) or ACVRL1 (HHT type 2) gene, with 3% to 5% having a mutation in the SMAD4 gene (combined syndrome of HHT and juvenile polyposis). The Curaçao diagnostic classification involves four criteria—recurrent and spontaneous epistaxis; multiple telangiectasias on the skin of hands or face, or inside the nose or mouth; AVMs or telangiectasias in one or more organs, including lungs, brain, liver, intestines, stomach, and spinal cord; and a family history of HHT in a first-degree relative—with three positive criteria required for a definite clinical diagnosis of HHT.
All patients with possible or confirmed HHT should undergo screening for AVMs in the lungs and vascular malformations in the brain because vascular abnormalities in these organs are associated with adverse outcomes. The current recommendation for the initial screening for pulmonary AVMs is a transthoracic contrast (bubble) echocardiogram, which shows the late entry of agitated saline from the right to the left side of the heart. If the echocardiogram is positive, this is followed by a chest CT scan with a pulmonary embolism (PE) protocol angiogram that detects the presence of pulmonary AVMs with high sensitivity. A chest radiograph will only suggest the presence of larger AVMs and miss smaller AVMs that still can be embolized (choice A is incorrect). All patients with possible or definite HHT should undergo screening for pulmonary AVMs.
The patient had an abnormal transthoracic contrast echocardiogram showing a right-to-left (late entry of agitated saline bubbles from the right to left side of the heart) shunt followed by a chest CT PE protocol angiogram that showed numerous pulmonary AVMs (Figures 1 and 2) that were subsequently identified at pulmonary angiography (Figure 3) and embolized by means of interventional radiology (Figure 4), with postembolization images showing successful embolization (Figure 5). Embolization is recommended for all AVMs that reasonably can be embolized, especially those with feeding vessels 3 mm or larger. Multidisciplinary expert care for patients with HHT is available at HHT Foundation International-accredited HHT Centers of Excellence. The patient underwent brain MRI, with and without contrast material, the results of which were normal. He will be followed up with periodic chest CT angiograms for the development of new AVMs.1
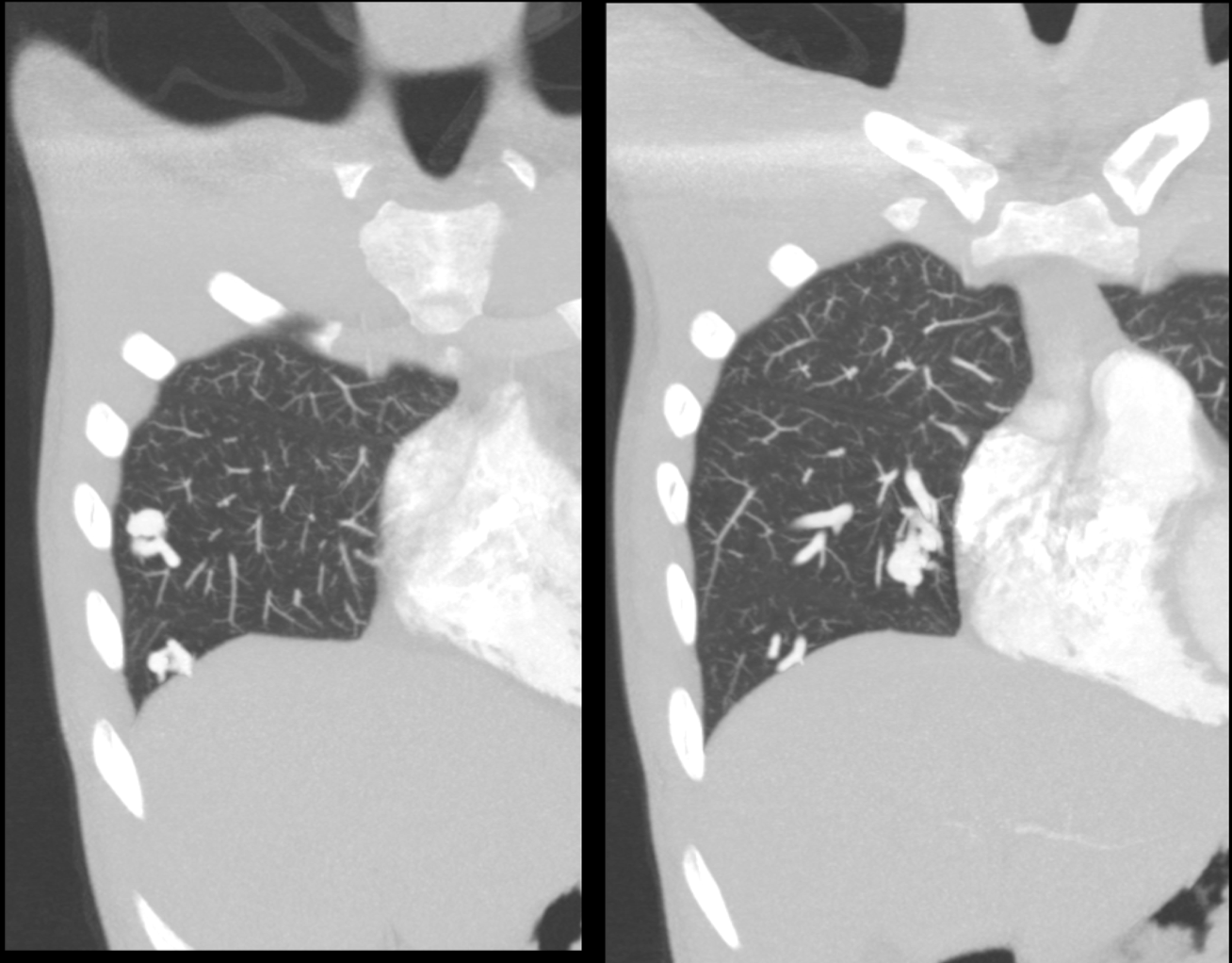
- Figure 1

- Figure 2
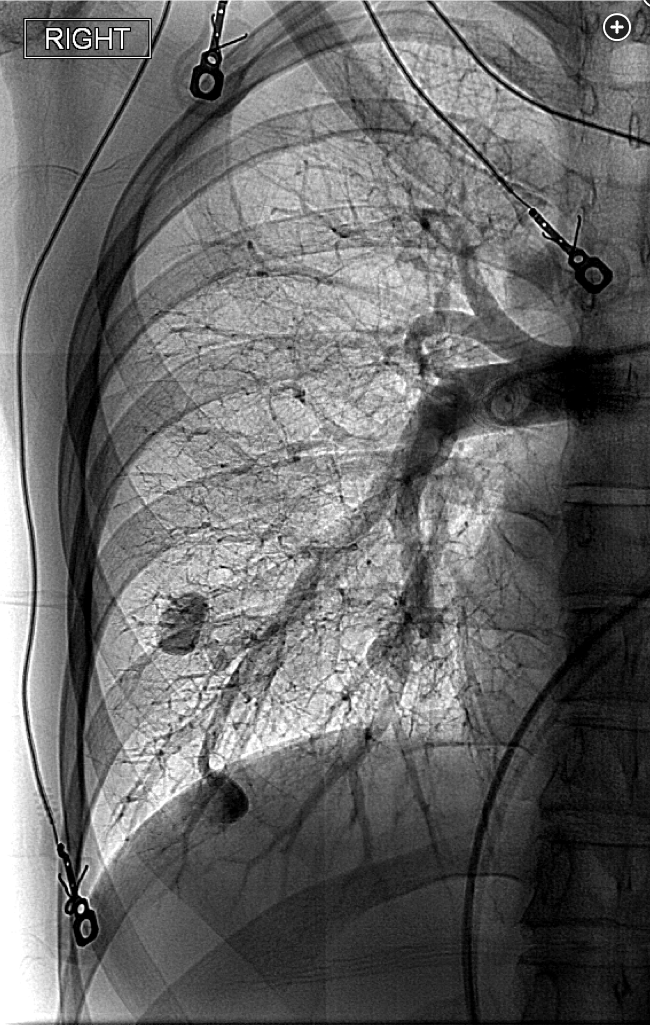
- Figure 3
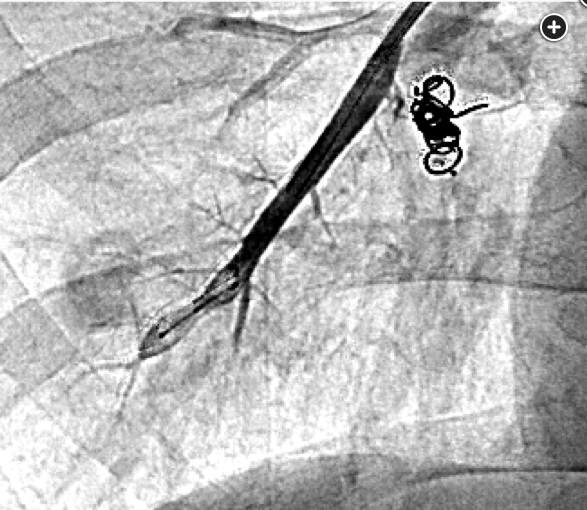
- Figure 4

- Figure 5