placental transmogrification of the lung
- related: Pulmonary Diseases
- tags: #literature #pulmonology
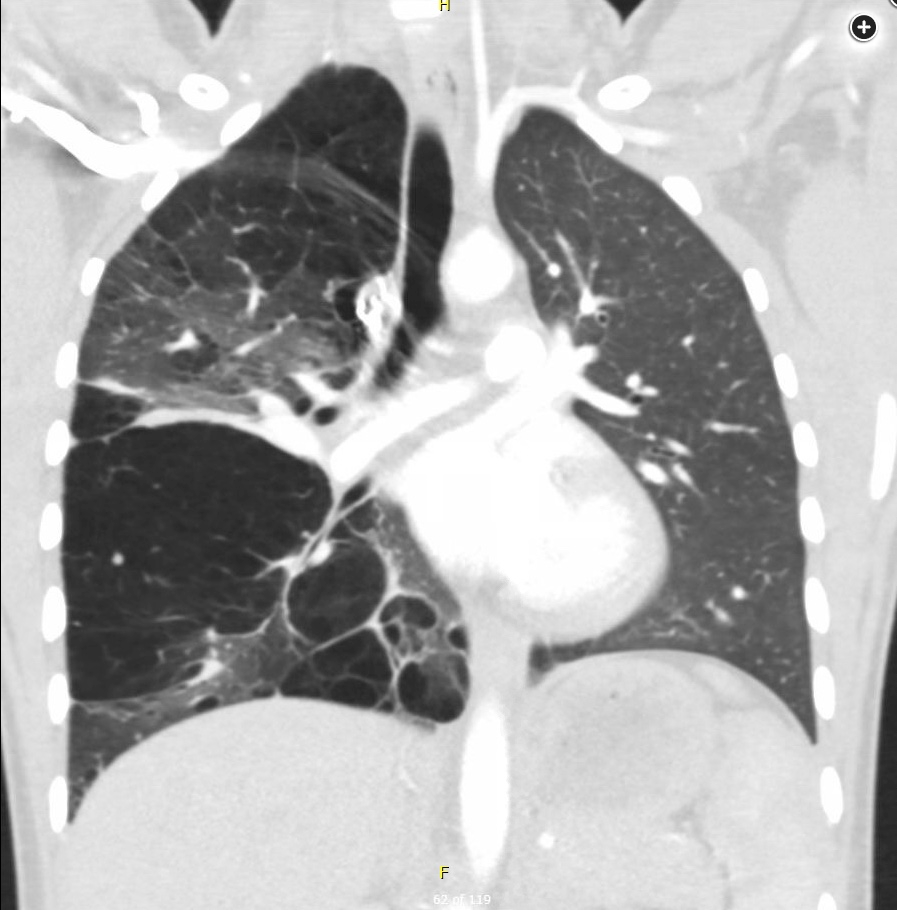
This patient was ultimately diagnosed with placental transmogrification of the lung (PTL), a rare benign cystic or bullous lesion of the lung that is considered as a histologic variant of unilateral bullous emphysema. PTL is histologically diagnosed on the basis of presence of papillary structures resembling placental villi. Patients with PTL often develop respiratory symptoms such as dyspnea, chest tightness, and cough. Initial management of unilateral bullous disease includes optimization of medical management with bronchodilators, inhaled corticosteroids, smoking cessation, and appropriate vaccinations (choice B is correct). As a later step if medical management fails to control symptoms, patients are often referred for surgical bullectomy (choice D is incorrect).
Despite recent travel, this patient has no other risk factors of pulmonary embolism, and CT pulmonary angiogram is low yield (choice C is incorrect). There is no pneumothorax visible on imaging and no indication for placement of a thoracostomy tube (choice A is incorrect).
Congenital lung malformations are rare but can cause significant morbidity; when unrecognized, they may lead to unwarranted intervention (eg, inappropriate placement of a chest tube in a patient with congenital lobar emphysema). Congenital lung malformations that may present as unilateral cystic or bullous lesions include bronchogenic cysts, congenital lobar emphysema, and Swyer-James-MacLeod (SJM) syndrome. Bronchogenic cysts (also called foregut duplication cysts) arise from abnormal budding of the foregut during development; they can be central or peripheral and filled with air or fluid.
Bronchogenic cysts may present with a wide variety of symptoms—including respiratory distress and feeding difficulty in newborns or coughing and wheezing that simulates asthma in the second decade of life—or may remain asymptomatic to adulthood. Bronchogenic cysts should be managed with surgical excision because there is potential for malignant degeneration.
Congenital lobar emphysema (CLE) is characterized by lobar hyperinflation that is the result of obstruction of the developing airway. Most cases present in infancy, although some may remain asymptomatic for years. Chest radiography typically demonstrates hyperinflation of the affected lobe with compression and atelectasis of the contralateral lung. Patients with CLE who are asymptomatic may be conservatively managed, as has been reported in multiple case series. Infants with respiratory distress due to CLE may need to undergo surgical resection of the affected lobe; they generally have good outcomes but may develop hyperinflation and pulmonary function test abnormalities later in life.
SJM syndrome is an uncommon cause of hyperinflation of one lung or one lobe that is thought to be a postinfectious form of bronchiolitis obliterans. Most patients with SJM are asymptomatic, but some may develop complications including bronchiectasis, lung abscess, and spontaneous pneumothorax. Management is generally conservative.1