pneumonia tularemia needs to be treated with aminoglycoside
- related: Pulmonology
- tags: #literture #pulmonology
Given the epidemiologic facts, clinical course, and pleural fluid findings, this patient is highly likely to be suffering from severe pneumonic tularemia, and the recommended treatment is with an aminoglycoside (choice A is correct).
Tularemia is a zoonotic infection caused by Francisella tularensis, a gram negative coccobacillus. Humans are infected either by direct contact with infected animals—typically rodents or vectors carrying the organism (ticks or mosquitoes). This infection has been reported in every state of the continental United States with the largest number of cases reported in the south central United States. In this case, the patient’s direct contact with small game at the time of butchering was the likely exposure.
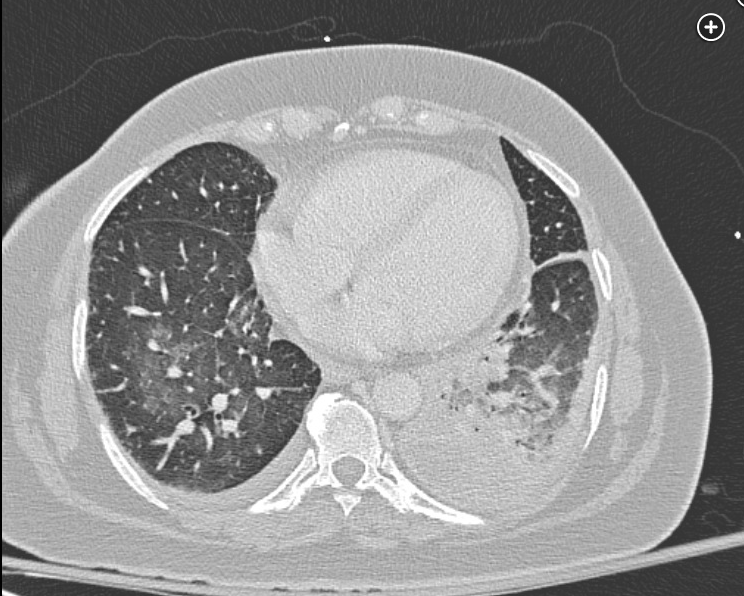
The clinical manifestations of tularemia vary from asymptomatic infection to septic shock and death. Initial symptoms are nonspecific and include fever, chills, malaise, headache, generalized body aches, abdominal pain, emesis, or diarrhea. When the portal of entry is the skin (Figure 4), an ulcer may be present (ulceroglandular tularemia), and in some patients, the suppurative lymphadenopathy is the most obvious finding (glandular tularemia). Ocular involvement has been described as well. When the organism is inhaled or spreads hematogenously, pharyngeal or pneumonic tularemia can occur, the latter signaling more severe disease. Lung infiltrates may be nodular in character and when pleural effusions develop, they often exhibit a lymphocytic predominance (as in this case). Pneumonic tularemia often presents as CAP with negative cultures and progression, despite empiric antibiotics, and when epidemiologic evidence supports this possibility, treatment for tularemia should be started pending serologies and culture. A systemic form of tularemia, so-called typhoidal disease, can also be seen. In these patients, skin, lymph node, and lung findings are absent. Finally, this organism is considered a category A bioterrorism agent and would likely be delivered as a weapon in aerosolized form with pneumonia as a prominent finding. The fact that tularemia could be a result of biowarfare mandates that confirmed cases are to be reported immediately to the Centers for Disease Control.
Diagnosis can be made by culture, although the organism is fastidious and difficult to recover in culture. Material that should be considered for culture include ulcer and lymph node drainage, blood, sputum, and pleural fluid. In this case, the pleural fluid cultures were positive after several days. Diagnosis in the proper context can also be made serologically by a four-fold rise in antibodies to the organism between acute and convalescent serum. but this testing may require 2-4 weeks or more.
Aminoglycosides are recommended treatment for severe tularemia. While historical use has usually involved streptomycin, gentamicin is recommended by many experts because serum levels can more readily be followed and the medication dose adjusted. Fluoroquinolones have significant activity against Francisella but are usually recommended for moderate disease, and this patient’s history of possible tendon rupture associated with an antibiotic would be a contraindication to their use. Aztreonam and the carbopenems are not recommended for treatment of tularemia.
Another unusual disease presenting as pneumonia is plague, caused by the gram negative bacillus Yersinia pestis. The organism is transmitted to humans from rodents by a flea. While tularemia is relatively rare in the United States, plague is extremely rare. In recent years, cases have been limited to the Western United States and, hence, the history here is inconsistent. The bacillus is also distinctive in its appearance microbiologically, with bipolar gram negative staining (“safety pin” appearance). Finally, an aminoglycoside would also be effective against this potential infection.1
