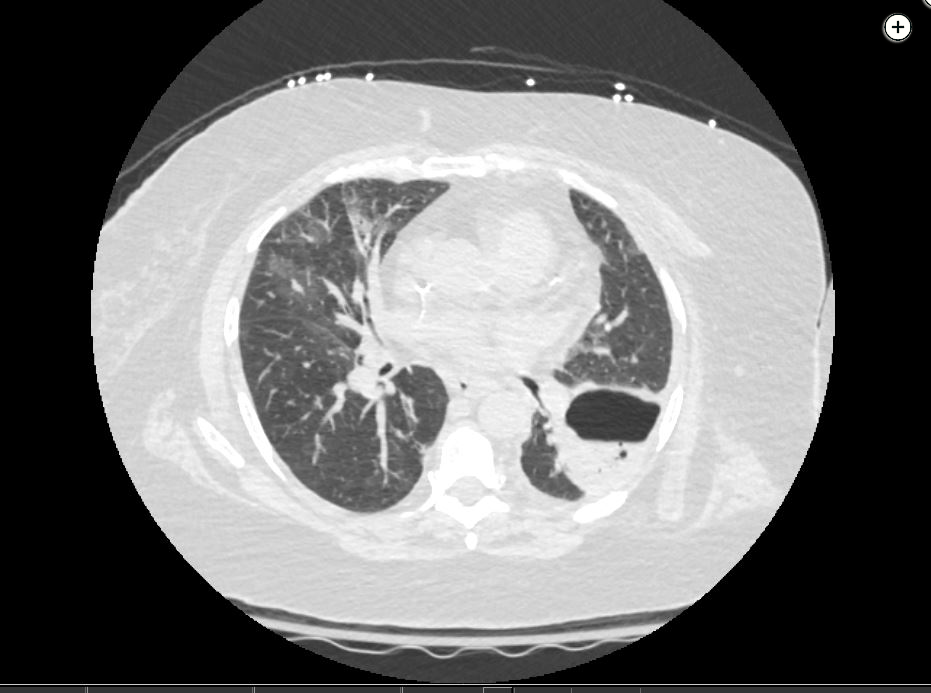
pulmonary abscess
- related: Pulmonology
- tags: #literature #pulmonology
Pulmonary abscess is a collection of pus within the lung parenchyma with confined cavitation that results from a pulmonary infection.
- Typical patient population:
- poor dentition
- homeless
- endocarditis with septic embolization
- IVDU
- impaired swallowing
- severe dementia
- old people
- altered consciousness
- Obtunded alcoholic
- seizure disorder
- poor dentition
Lung abscesses may also form as a consequence of septic embolization, direct extension of an empyema, endobronchial obstruction from a foreign body or tumor, or superinfection of damaged lung tissue (eg, contusion or infarct).
The three bacterial causes of pulmonary abscesses are:
- Staphylococcus aureus in IV drug users with endocarditis.
- Klebsiella pneumoniae in obtunded alcoholics.
- Anaerobic oral flora in patients with aspiration pneumonia
Bacteria from the oropharynx implicated in pulmonary abscesses from aspiration include:
- Bacteroides
- Fusobacterium
- Peptococcus
Foul smelling sputum in a patient with aspiration is indicative of anaerobic infection.
Treatment
- antibiotics for 4-6 weeks
- Chest imaging follow up
- avoid putting chest tube or drain into pulmonary abscess
- increases risk of bleeding
- can contaminate pleural space and leads to empyema
A small percentage of patients fail antimicrobial therapy and require procedural intervention. Percutaneous catheter drainage or transbronchoscopic catheter drainage may be considered for patients who do not respond to antibiotic therapy, depending on the location of the abscess (peripheral/abutting the pleura vs central), but should not be attempted prior to antibiotic therapy. Surgical intervention is rarely indicated for patients who fail to improve with antibiotic therapy or develop a complication during treatment (eg, bronchopleural fistula). Mortality with surgical intervention is as high as 15% to 20%, and surgery should not be considered before a prolonged trial of antibiotic therapy.123
Complications
- risk of rupture into the airway or pleural space
Links to this note
-
pulmonary cavitary lesions do not need anaerobic coverage vs abscess
- abscess do need anaerobic coverage: patients with abscess usually have anaerobic bacteria from aspiration (pulmonary abscess)