thoracic endometriosis syndrome TES can cause catamenial pneumothorax and hemothorax
- related: Pulmonary Diseases
- tags: #literature #pulmonology
The most likely diagnosis in this patient is thoracic endometriosis syndrome (TES) (choice A is correct). TES includes four well-recognized clinical entities: catamenial pneumothorax, catamenial hemoptysis, catamenial hemothorax, and lung and pleural nodules. This patient presented with a catamenial hemothorax and was found to have lung and pleural nodules on CT scanning (Figure 4). Additionally, the pleural biopsy shows findings compatible with endometriosis of the pleura (Figure 5). Endometriosis refers to the presence of endometrial tissue outside the uterine cavity and myometrium. It has been identified in virtually all tissues and organs in the female body with the exception of the spleen, which seems to resist implantation of endometrial tissue. Endometriosis is rare before menarche and after menopause, when women are deficient in estrogen. The distribution of endometrial implant through the diaphragm seems to be asymmetric, with the right being affected more than the left. As seen in this case, the diffusion of endometrial cells through fenestrations is evident in the literature because of an identical preponderance of right-sided lesions of both the diaphragm and pleura.
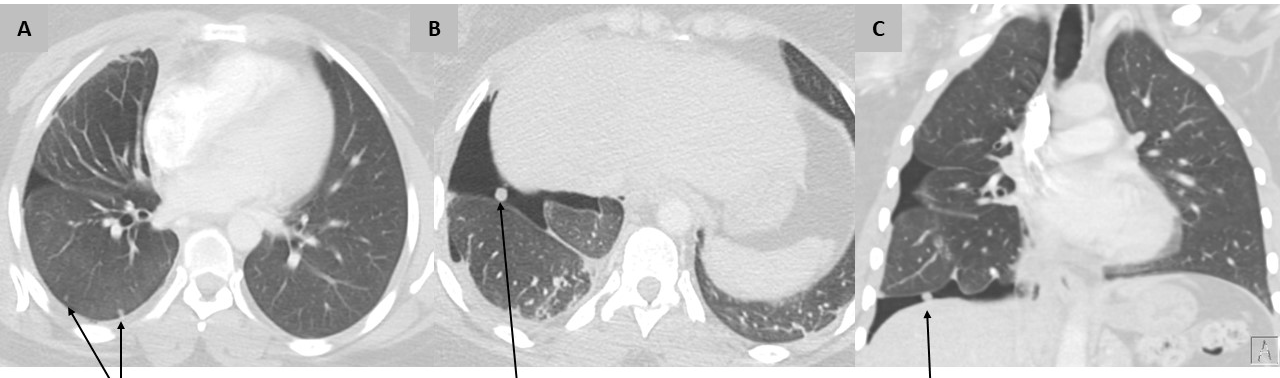
- Chest CT scans of thoracic endometriosis syndrome. A. Axial view shows pulmonary micronodules and a pneumothorax. B. Axial view shows pleural-based, diaphragmatic nodule and a pneumothorax ex vacuo. C. Coronal view shows pleural-based, diaphragmatic nodule and a pneumothorax ex vacuo.
In a retrospective review of 110 cases of TES, the predominant clinical presentation was pneumothorax in 79 (72%) patients, hemoptysis in 16 (14%), hemothorax in 13 (12%), and lung mass in two (2%). The mean duration of symptoms before the diagnosis of TES was 15 ± 2.4 months. Symptoms are generally cyclical, occurring within 24 to 48 h after menses. The most sensitive tests for detection of pneumothorax and hemothorax are chest radiographs and CT scanning, whereas MRI is preferable for the detection of diaphragmatic endometriosis, with a reported sensitivity of 78% to 83%. Other manifestations of TES that may be present on CT scans include ground-glass infiltrates, thin-walled cavities, pleural and pulmonary nodules, bullous formation, bronchial wall thickening, as well as pneumomediastinum and pneumoperitoneum. Bronchoscopy rarely produces a tissue diagnosis, although it may be helpful in the assessment and treatment of hemoptysis or in excluding other pulmonary pathologic findings. Pleural fluid cytologic studies are rarely diagnostic. The gold standard for establishing a definitive diagnosis of diaphragmatic endometriosis is video laparoscopy and video-assisted thoracoscopic surgery.
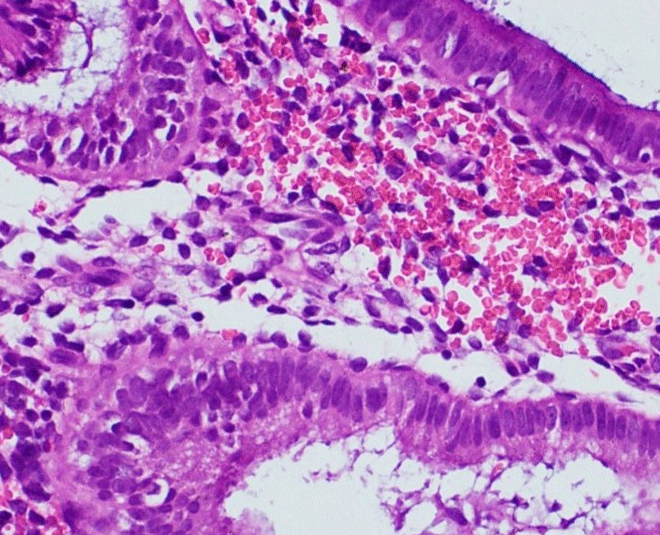
- Pleural biopsy specimen: hematoxylin and eosin–stained tissue (×40 magnification) shows well-formed endometrial glands lined by a columnar epithelium, surrounded by endometrial-type stroma.
The optimal management of endometriosis is controversial because current evidence is derived from case reports and small clinical series. Surgery, hormonal treatments, and combined approaches have all been proposed, with variable results in terms of short-term and long-term outcomes. Endometrial tissue is completely dependent on estrogen for continued growth, so effective therapy for endometriosis requires hormonal suppression of estrogen production by the ovaries or surgical ablation of endometrial lesions. Hormonal suppressive therapy can be accomplished surgically or medically by using oral contraceptives, danazol, or gonadotropin-releasing hormone analogues. Birth control pills are used most commonly, but there is a high recurrence rate (50%). Gonadotropin-releasing hormone agonists suppress gonadotropin secretion and desensitize the ovarian response to gonadotropin to achieve hypoestrogenemia. This is accomplished without androgenic side effects.
Although metastatic breast cancer can present with large, malignant pleural effusion, as well as pulmonary and pleural nodules, a hemothorax is exceedingly rare. Furthermore, the histopathology is inconsistent with metastatic carcinoma (choice B is incorrect). In patients with hereditary hemorrhagic telangiectasia, hemothorax can result from intrapleural rupture of pulmonary arteriovenous malformations. However, the CT scanning and histologic findings in this case do not support this diagnosis (choice C is incorrect). Similarly, although hemothorax has been described as a rare complication of intrathoracic extramedullary hematopoiesis, the CT scanning and histologic findings are not consistent (choice D is incorrect).1