transplant associated thrombotic microangiopathy
- related: Hematology
- tags: #literature #hemeonc
This patient has a clinical syndrome most consistent with transplant-associated thrombotic microangiopathy (TMA), a rare but serious complication of bone marrow and hematopoietic stem cell transplant. Risk factors for transplant-associated TMA include the use of calcineurin inhibitors, mammalian target of rapamycin inhibitors, graft-vs-host disease, multiple previous transplants, human leukocyte antigen mismatch, opportunistic infection, and certain conditioning regimens (especially those including total body irradiation).
Clinical features of transplant-associated TMA include new or worsening hypertension, progressive acute kidney injury, worsening thrombocytopenia, microangiopathic hemolytic anemia, pulmonary hypertension, and progressive neurologic dysfunction. Transplant-associated TMA often does not respond to traditional management strategies such as drug discontinuation and plasma exchange. Rituximab, defibrotide, and eculizumab may be beneficial, on the basis of case reports and retrospective case series, although further evidence is needed to support routine use in this high-risk clinical setting.
Early complications of hematopoietic stem cell transplant can involve virtually every organ system. Acute graft-vs-host disease typically manifests around the time of engraftment and usually involves the skin (maculopapular rash, which can become confluent and slough) and GI tract (diarrhea, abdominal pain, and liver function abnormalities with a cholestatic pattern), which are not prominent features of this presentation.
Engraftment syndrome is associated with systemic inflammation and characterized by fever, rash, and diffuse capillary leak, with resulting pulmonary edema and end-organ dysfunction. Acute kidney injury can occur, but microangiopathic hemolytic anemia findings are not common.
Diffuse alveolar hemorrhage is a rare complication of hematopoietic cell transplant most commonly occurring in association with certain conditioning regimens, pulmonary infections, and prolonged cytopenias (DAH can develop following stem cell transplant). It is also not typically associated with the multiple systemic abnormalities identified in this case.1234
A 66-year-old patient is transferred to the ICU for management of multiple complications from allogenic hematopoietic stem cell transplant for acute myelogenous leukemia. The patient is currently day +16, with delayed engraftment, persistent cytopenias, severe mucositis and a recent neutropenic fever treated with vancomycin and cefepime. The clinical course over the past several days has included new-onset delirium, worsening hypertension, and progressive acute kidney injury despite targeted crystalloid resuscitation, pain management, and treatment with multiple antihypertensives.
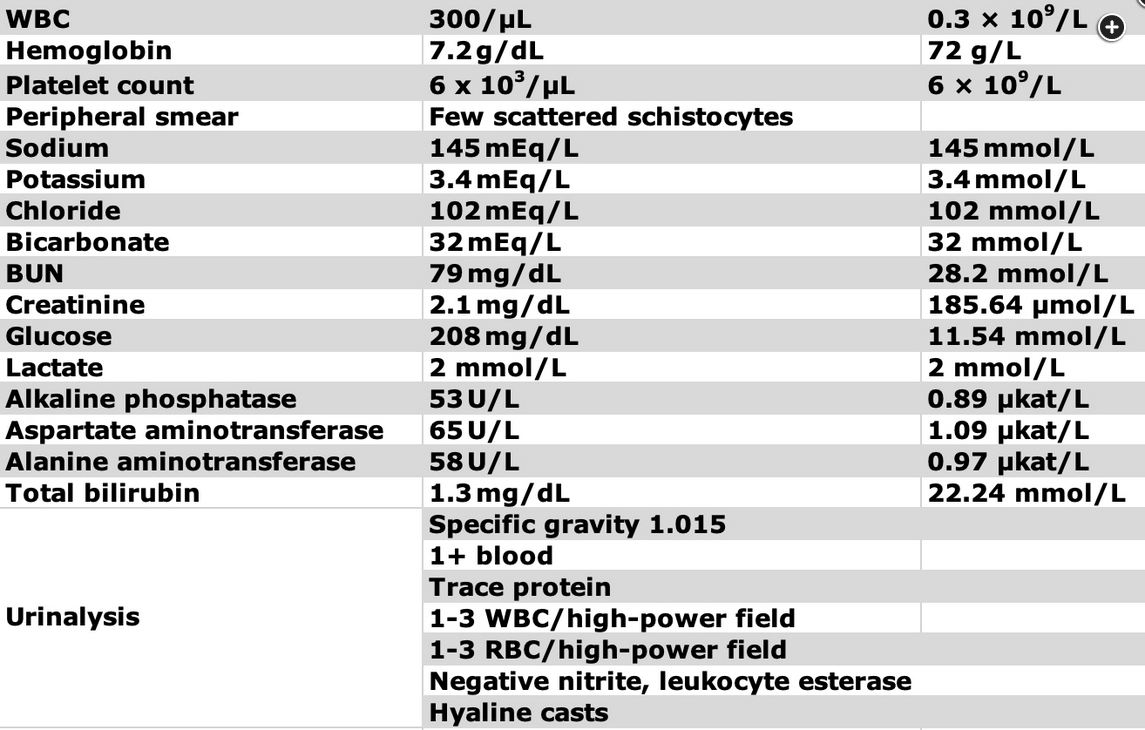
The temperature is 38.2°C, heart rate is 94/min, BP is 183/98 mm Hg, respiratory rate is 22/min, and Spo2 is 94% with the patient receiving 2 L/min supplemental oxygen. The patient is arousable but disoriented and ill appearing. Physical examination results are clinically significant for severe oropharyngeal mucositis; diminished bilateral breath sounds with scattered crackles; and a mildly distended, nontender abdomen. There are a few petechiae, 1+ bilateral lower extremity edema, and a right-side chest wall port without erythema or tenderness. Current laboratory test results are displayed in Figure 1. A chest radiograph demonstrates low lung volumes with mild patchy bilateral infiltrates.
Which diagnosis is most likely based on this clinical presentation?
Links to this note
Footnotes
-
Scully M, Cataland S, Coppo P, et al; International Working Group for Thrombotic Thrombocytopenic Purpura. Consensus on the standardization of terminology in thrombotic thrombocytopenic purpura and related thrombotic microangiopathies. J Thromb Haemost. 2017;15(2):312-322. PubMed ↩
-
Weitz IC. Thrombotic microangiopathy in cancer. Semin Thromb Hemost. 2019;45(4):348-353. PubMed ↩
-
Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for treatment of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2496-2502. PubMed ↩