traumatic pulmonary pseudocysts can result following trauma
- related: Pulmonology
- tags: #literature #pulmonology
- well rounded, thin wall, maybe air/fluid, usually content is hemorrhagic and thus can be hyperattenuating (whiter) on CT.
- other ddx includes septic emboli, cavitary lesions
- management includes observation and repeat imaging
Source
This patient has traumatic pulmonary pseudocysts (TPP), a condition which—if uncomplicated—is managed with observation and repeat chest imaging (choice C is correct). TPP are rare manifestations of blunt or nonpenetrating thoracic trauma that develops through a mechanism allowing transmission of high compressive forces to the lung parenchyma. The pathogenesis of TPP is related to the shear forces often experienced during blunt trauma as can occur following a motor vehicle accident. Compression of the chest wall, followed by rapid elastic recoil, results in laceration of alveoli and bronchioles with subsequent air-filling and formation of confluent pulmonary cavities. These cavities may fill with hemorrhagic material from surrounding alveolar capillaries or pulmonary vessels. Due to absence of a true epithelium, these structures are more commonly referred to as “pseudocysts.”
TPP have been reported in infants, children, and adults; however, the majority seem to occur in individuals less than 30 years of age, with a male predominance. The proposed mechanism is similar despite differences in body size; however, the manifestations tend to be most pronounced in younger individuals due to the compliance of their chest walls, which permits greater transmission of the force of impact to the lung parenchyma. The usual clinical manifestations may include cough, dyspnea, hemoptysis, chest pain, fever, and leukocytosis.
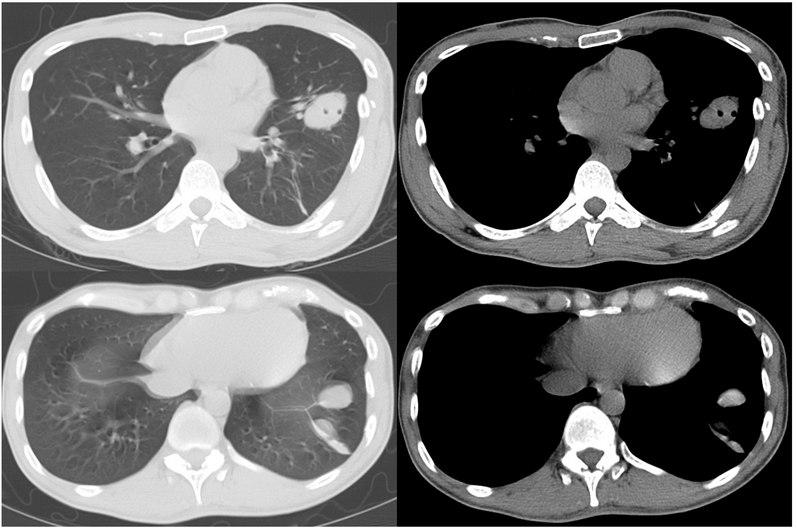
On chest CT, TPP appear as well-defined, oval, or spherical shaped, thin-walled cavities within the lung parenchyma that are filled with fluid and/or air. Their size can vary between 1 and 14 cm, and they may be focal or multifocal, as well unilateral or bilateral, though are more commonly seen in the lower lobes. The fluid content of the cavities is hemorrhagic, originating from surrounding alveolar capillaries or pulmonary vessels. The main mechanism is compression and tearing of the lung parenchyma at the site of impact (it may also occur contralaterally or “contre-coup”) against osseous structures, rib fractures, or preexisting pleural adhesions. The high sensitivity of CT, as well as their increased use in trauma patients, has raised the frequency of TPP detection.
The management of uncomplicated TPP consists of close observation and serial imaging to ensure resolution. Of note, one of the nonenhanced soft tissue CT images in this patients demonstrates hyperattenuation within one of the lesions, suggestive of its hemorrhagic content (Figure 2).
Bronchoscopy with BAL would be of minimal value in a nonimmunocompromised patient with such nodular opacities (choice A is incorrect). Based on the patient’s clinical presentation and previously outlined radiographic findings, a transthoracic CT-guided biopsy would not be indicated (choice B is incorrect). Although septic pulmonary emboli (SPE) may be a consideration in a patient with a history intravenous drug presenting with coexisting cavitary and noncavitary pulmonary nodules (peripheral nodules at varying stages of evolution), our patient’s clinical and laboratory findings, as well as the morphological characteristics of the lesions on CT, are not suggestive; therefore, there is no indication to pursue to transesophageal echocardiography (choice D is incorrect).1