use CTA to look for large vessel occlusion in ischemic stroke patients
- related: Neurology, use CTA neck to assess for blunt cerebrovascular injury
- tags: #literature #icu #neuro
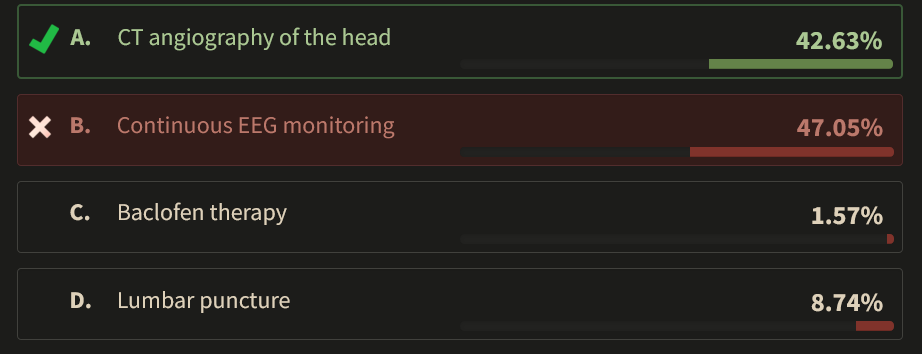
This patient has signs and symptoms of brainstem ischemia. The absence of cranial nerve functions, myoclonic movements at the time of onset of symptoms, and early hyperreflexia are all suggestive of brainstem involvement. The CT scan (Figure 1) shows subtle signs of hypodensities in her brainstem and cerebellum. A quick trick for looking at CT scans for subtle ischemia is to change the contrast of the image to accentuate the difference between ischemic and nonischemic tissue or to view the image from farther away, which allows the eye to discriminate changes in density better.
Causes of stroke in the young include coagulopathies, vasculitides, certain drug intoxications such as cocaine, and vertebral dissections (particularly from trauma). Given the history, the most likely of these is a traumatic dissection. It is important to note that although the dissection occurs at the time of the injury, clots can form on the denuded tissue and embolize later. Regardless of the cause, the best hope she has for improvement is to reestablish blood flow; therefore, determination of whether she has a large vessel occlusion amenable to endovascular intervention is critical. A CT angiogram is therefore the most important intervention. Brainstem ischemia is often amenable to intervention even after hours have elapsed. Patients should be considered for intervention up to 24 h after stroke symptom onset unless there are signs of hemorrhage or herniation.
Patients with brainstem ischemia often have tonic reactions associated with loss of consciousness at the onset. These may also include myotonic movements that can be confused for seizures. Continuous EEG would help determine whether these movements were seizures or myoclonus, but this is a secondary issue that should be addressed after the question of potential revascularization is addressed.
Although the patient has increased tone and hyperreflexia on examination, this is the result of her brainstem injury, which should be the focus of the treatment. Symptom therapies such as baclofen should be considered later, once the underlying cause of the neurologic injury or process is determined.
Likewise, lumbar puncture is an appropriate test to investigate the causes of acute comatose syndromes, but this is a clear example of brainstem ischemic injury, which cannot be diagnosed with lumbar puncture. Other entities for which a lumbar puncture could be beneficial in diagnosis are farther down the differential diagnosis. In addition, if there is significant swelling of the brainstem, lumbar puncture is contraindicated because it may lead to herniation; the brainstem forms a “cork” in the foramen magnum that is then moved by suction when the lumbar spinal pressure is suddenly decreased.
A 38-year-old woman presents with seizures and hypertension. According to family, she was involved in a motor vehicle collision (MVC) 2 days previously. She did not have any injuries or symptoms at the time of the MVC, and her family reports that she has not reported any problems over the last 2 days. Today, she was found on the ground by her family, with stiffening and extension of the arms and legs followed by occasional rapid jerking of her arms and legs. The patient did not return to consciousness after these movements. She was brought to the emergency department by emergency medical services, where she underwent intubation, and CT scanning of the head was performed (Figure 1). She was then transferred to the ICU. 123
At the time of ICU admission, she is intubated and is unarousable without any sedating medications. Her temperature is 37.8 °C, heart rate is 65/min, and BP is 190/85 mm Hg. The neurological examination results are significant for decreased pupillary constriction velocity bilaterally and absent corneal responses. She has increased tone and tendon reflexes in her arms and legs. She is not able to cooperate with any of the examination.
What is the most appropriate next step?
Links to this note
Footnotes
-
Salerno A, Strambo D, Nannoni S, et al. Patterns of ischemic posterior circulation strokes: a clinical, anatomical, and radiological review. Int J Stroke. 2022;17(7):714-722. PubMed ↩
-
Tao C, Nogueira RG, Zhu Y, et al; ATTENTION Investigators. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. 2022;387(15):1361-1372. PubMed ↩