vaccine induced immune thrombotic thrombocytopenia VITT
- related: Hematology
- tags: #literature #icu
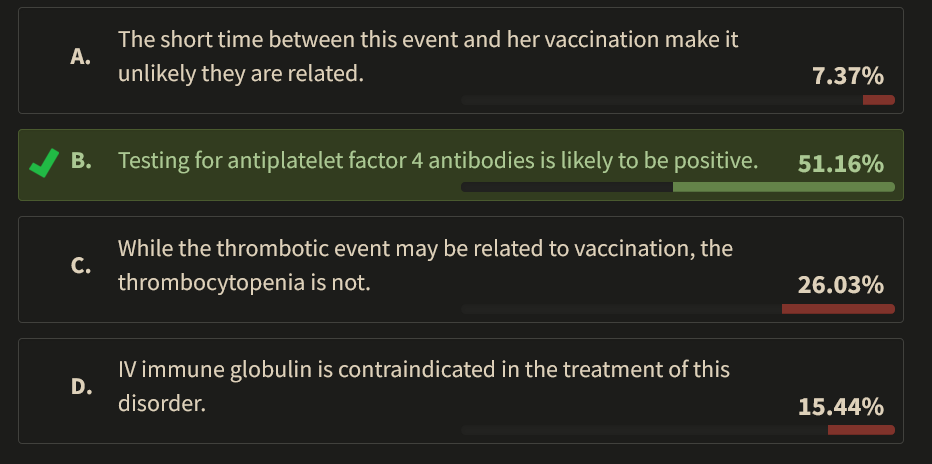
The patient described is likely suffering from vaccine-induced immune thrombotic thrombocytopenia (VITT), also termed thrombosis with thrombocytopenia syndrome and vaccine-induced prothrombotic immune thrombocytopenia. This syndrome shares many features with heparin-induced thrombocytopenia (HIT), including positive testing for antibodies recognizing platelet factor 4.
VITT was first described in individuals receiving the ChAdOx1 nCoV-19 vaccine (AstraZeneca, University of Oxford, and Serum Institute of India) and subsequently in those receiving the Ad26.COV2.S vaccine (Janssen [Johnson & Johnson]). It is an extremely rare complication of vaccination and appears largely, if not entirely, limited to adenoviral vector-based vaccines. Nonetheless, because many millions of individuals have been vaccinated, it is a condition that clinicians may encounter. It is important to note that in all risk-benefit analyses, the risk of clotting or bleeding disorders is many times greater from COVID-19 infection itself than from coagulopathic reactions to these vaccines. VITT is caused by IgG antibodies that recognize platelet factor 4, as in HIT, but the epitope recognized is different from that recognized in HIT. The syndrome typically appears 5-10 days after vaccination.
Thrombocytopenia, usually in the range of 50 x 103/μL (50 x 109/L), is commonly present. Both arterial and venous thrombosis may occur, but by comparison with HIT, there is a disproportionate fraction of patients with cerebral (as in our patient) or splanchnic vein involvement. A mnemonic has been proposed to heighten suspicion for VITT: vaccine given, interval consistent (5-30 days after vaccination), thrombosis, and thrombocytopenia. This patient met all of these criteria. An absence of exposure to heparin and a positive test by enzyme-linked immunosorbent assay for antiplatelet factor 4 antibodies are considered confirmatory. The patient described had a high titer of platelet factor 4 antibodies. When thrombosis due to VITT has occurred, anticoagulation is required. Soon after recognition of the syndrome, some authorities cautioned against the use of heparin-based treatment because of the similarities to HIT, but growing information about the differences in the immunology of antibody generation in the two disorders has altered this approach. Some still prefer early use of an oral direct thrombin inhibitor, fondaparinux, argatroban, or bivalirudin. Given how rapidly understanding of this syndrome is changing, consultation with specialists in clotting disorders is recommended. Most patients should also receive IV immune globulin during the acute phase of their illness to block VITT antibody-induced platelet activation.
A 28-year-old female nursing student is admitted to the ICU for obtundation following a seizure treated in the ED. One day ago, she experienced a severe headache that was unresponsive to acetaminophen. Today, her family observed a generalized tonic-clonic seizure, and emergency medical services were summoned. She was obtunded en route to the hospital and then had another generalized seizure during her initial evaluation by emergency medicine staff. Her seizure responded to IV lorazepam, and she was loaded with IV levetiracetam. Her laboratory studies in the ED were remarkable only for a platelet count of 62 x 103/μL (62 x 109/L). Neuroimaging after she was stabilized included magnetic resonance venography, which revealed a superior sagittal sinus thrombosis. The patient’s family describes her to be in excellent health, having never been hospitalized and taking no medications. Three months ago, on entry to nursing school, a general exam was normal as was a complete blood count. One week ago, she received an adenoviral vector-based vaccine and had no adverse reaction. 12345
Which of the following is most likely true about this patient’s thrombotic event?
Links to this note
Footnotes
-
Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021;384(22):2092-2101. PubMed ↩
-
Huynh A, Kelton JG, Arnold DM, Daka M, Nazy I. Antibody epitopes in vaccine-induced immune thrombotic thrombocytopaenia. Nature. 2021;596(7873):565-569. PubMed ↩
-
Schultz NH, Sørvoll IH, Michelsen AE, et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med. 2021;384(22):2124-2130. PubMed ↩
-
Tiede A, Sachs UJ, Czwalinna A, et al. Prothrombotic immune thrombocytopenia after COVID-19 vaccination. Blood. 2021;138(4):350-353. PubMed ↩