very high WBC can cause false hypoxemia leukocyte larceny
- related: Oncology
- tags: #literature #icu #oncology
The patient’s findings are of spurious or factitious hypoxemia, sometimes referred to as “leukocyte larceny.” In this circumstance, oxygen consumption by actively metabolizing WBCs results in depletion of dissolved plasma oxygen during transport of the arterial specimen to the laboratory. The degree of reduction in plasma dissolved oxygen is associated with the number of WBCs present, duration of time between obtaining the specimen and performance of the analysis, and temperature of the specimen. WBC counts >100,000/µL (>100 × 109/L) are commonly associated with factitious hypoxemia and counts >200,000/µL (>200 × 109/L) invariably demonstrate the finding.
This patient’s WBC count >900,000/µL (>900 × 109/L) should be expected to demonstrate substantial leukocyte larceny. Oxygen depletion can be mitigated either by placing the specimen immediately on ice for transport, thereby reducing WBC metabolism and oxygen consumption, or by analyzing the specimen immediately on obtaining it, although both options may be incompletely effective. The latter can be accomplished via point-of-care blood gas measurement. Inhibition of WBC oxygen consumption by addition of 0.77-molar potassium cyanide to the specimen is also effective in experimental conditions; however, potassium cyanide exposure can be highly toxic, and this technique is best performed under a fume hood. Of interest, all studies demonstrate that arterial PaCO2 is less affected by WBCs than is PaO2.
Carbon monoxide toxicity results in factitiously high SpO2 but does not alter arterial PaO2. Oxygen delivery by heated, humidified high-flow nasal cannula can successfully reverse severe hypoxemia in many cases, but this patient’s SpO2 value does not support use of the modality and suggests that arterial blood gas results are spurious. Normal chest radiography is common in patients with pulmonary embolism. However, the discrepancy between SpO2 and PaO2 should be resolved before actions based on the PaO2 results are taken.
This patient’s acute central retinal vein occlusion was also thought to be related to the very high WBC count, with altered blood rheology. After treatment to reduce his WBC count to <100,000/µL (<100 × 109/L), his PaO2 increased to 87 mm Hg while breathing room air.1234
A 53-year-old man is admitted with sudden onset of blurred vision and evidence of right central retinal vein occlusion. He reports dyspnea with exertion but reports no chest pain or cough. Chest radiograph is shown in Figure 1. Vital signs are a BP of 110/57 mm Hg, pulse rate of 110/min, respiratory rate of 22/min, temperature of 37.3 °C, and SpO2 of 99%. Serum chemistries are normal except for a potassium of 3.2 mEq/L (3.2 mmol/L).
CBC count reveals hemoglobin of 5.8 g/dL (58 g/L), hematocrit of 19% (0.19), platelet count of 34 × 103/μL (34 × 109/ L), and WBC count of 950,000/μL (950 × 109/L).
Arterial blood gas reveals pH of 7.42, PaCO2 of 38 mm Hg, and PaO2 of 28 mm Hg while breathing ambient air.
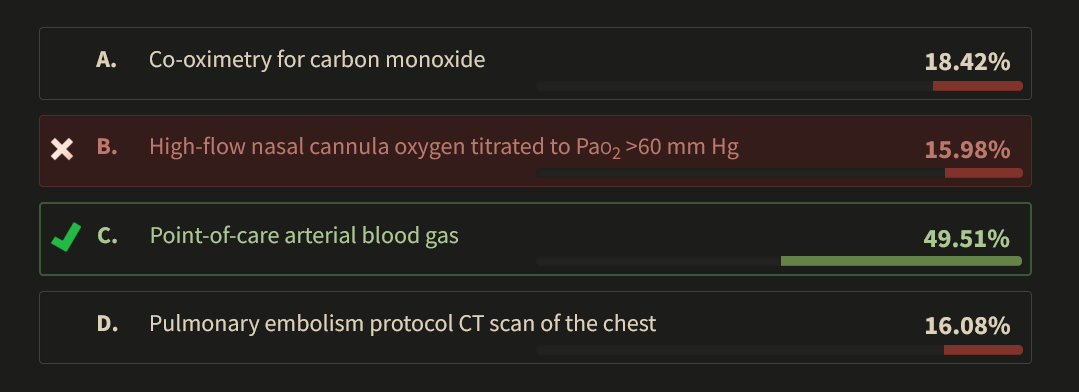
Which of the following is the most appropriate next step?
Links to this note
-
acute leukemia and hyperkeukocytosis
- pseudohypoxemia and pseudohyperkalemia: so many cells in blood samples drawn up that gobble up all oxygen = artificially low PaO2 than SpO2 on monitor. Lysis in the sample leads to artificially high K. (very high WBC can cause false hypoxemia leukocyte larceny)
Footnotes
-
Chillar RK, Belman MJ, Farbstein M. Explanation for apparent hypoxemia associated with extreme leukocytosis: leukocytic oxygen consumption. Blood. 1980;55(6):922-924. PubMed ↩
-
Fox MJ, Brody JS, Weintraub LR. Leukocyte larceny: a cause of spurious hypoxemia. Am J Med. 1979;67(5):742-746. PubMed ↩
-
Van de Louw A, Desai RJ, Schneider CW, et al. Hypoxemia during extreme hyperleukocytosis: how spurious? Respir Care. 2016;61(1):8-14. PubMed ↩