aspergillosis
- related: Infectious Disease ID, Allergic bronchopulmonary aspergillosis ABPA
- tags: #literature #pulmonology
Aspergillus
- most common species: A. fumigatus, A. flavus, A. niger, and the amphotericin-resistant A. terreus.
- Aspergillus produces disease after inhalation of airborne spores (90%) and only occasionally by traumatic skin inoculation. Of all the fungi, Aspergillus is notable for the diverse settings in which it can occur and the various clinical manifestations it can produce.
Types
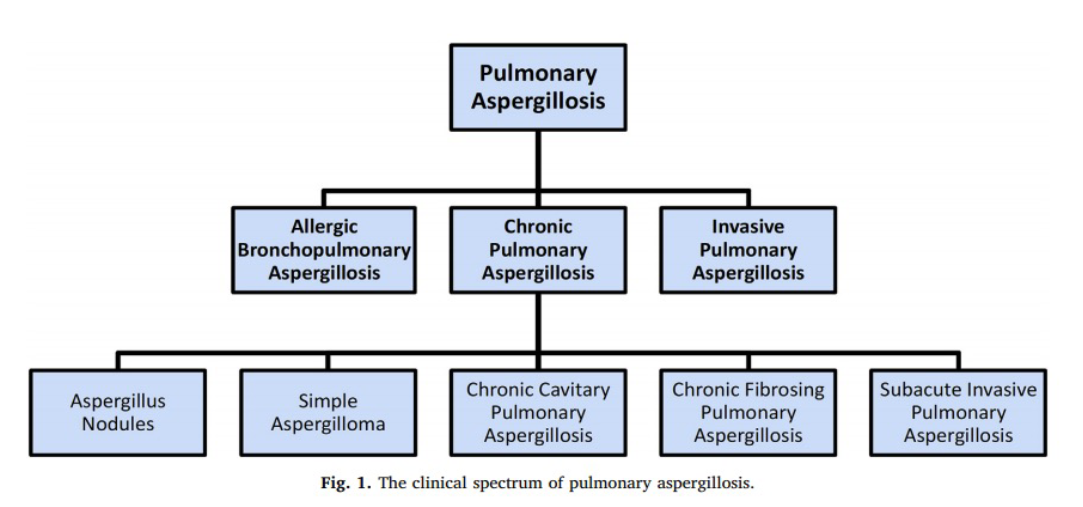
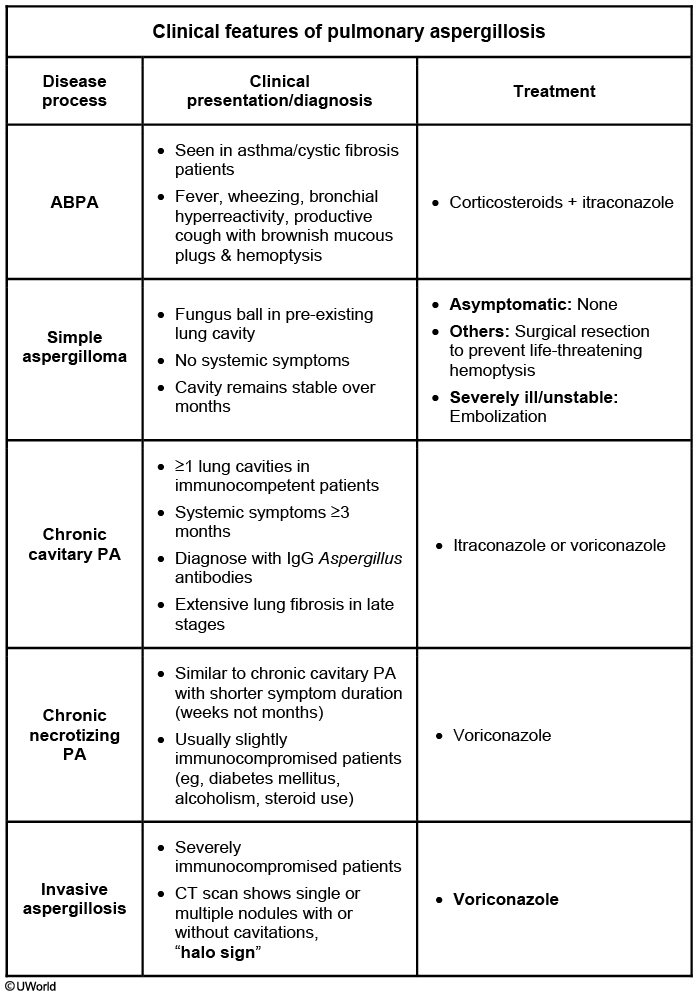
This patient most likely has invasive pulmonary aspergillosis (IPA). Aspergillus has diverse presentations, including asymptomatic infection in immunocompetent hosts, allergic bronchopulmonary aspergillosis (ABPA) in patients with asthma or cystic fibrosis, and various patterns of chronic PA. Risk factors for chronic PA include prior lung disease such as pulmonary tuberculosis, ABPA, lung cancer, chronic obstructive pulmonary disease, and sarcoidosis.
Symptoms of IPA are nonspecific and usually mimic bronchopneumonia: fever unresponsive to antibiotics, cough, sputum production, and dyspnea. Patients may also present with pleuritic chest pain (due to vascular invasion leading to thromboses that cause small pulmonary infarcts) and hemoptysis, which is usually mild. IPA is one of the most common causes of hemoptysis in neutropenic patients. Chest x-ray may not detect early-stage disease (ie, small nodules). Chest computed tomography (CT) scan shows single or multiple nodules with or without cavitations and “halo sign” (nodules surrounded by ground-glass infiltrates). Diagnosis is suggested by culture and histology.
Enzyme-linked immunosorbent assay on serum or bronchoalveolar lavage fluid can be used to detect galactomannan antigen (present in Aspergillus cell walls), especially in patients with hematologic malignancies. Voriconazole has become the gold standard as primary therapy for invasive aspergillosis. Voriconazole was more effective than amphotericin B as initial therapy for IPA and was associated with significantly improved survival (71% vs 58%, respectively) in a randomized trial (Choice A).
Invasive pulmonary aspergillosis
chronic cavitary pulmonary aspergillosis
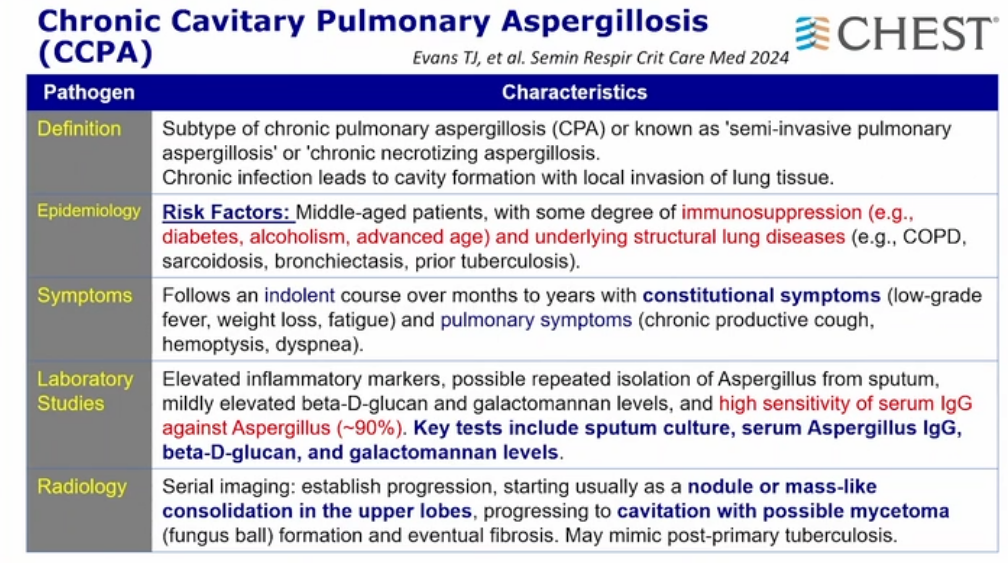
- aspergillosis invades space damaged by something else
- IgG, not IgE must be used for diagnosis
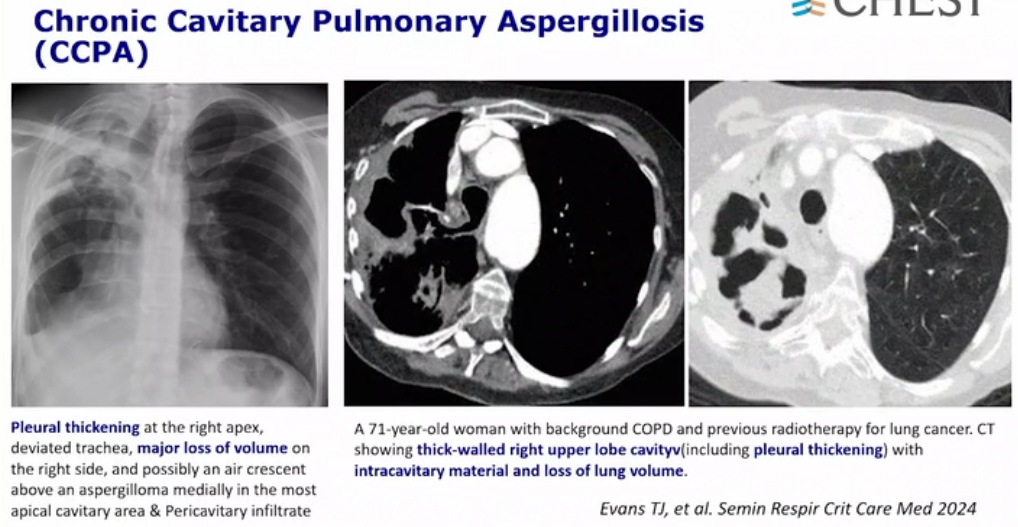
- previous space with now with pleural thickening
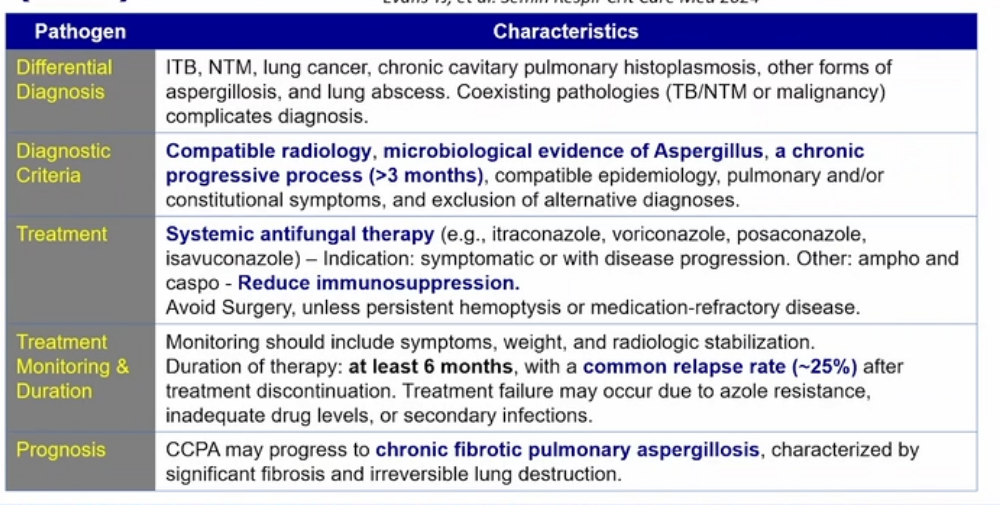
- must be there for more than 3 months
- itraconazole and reduce immunosuppression
- monitor treatment for 6 months Other forms of Aspergillus infection occur in different clinical settings. Chronic necrotizing aspergillosis is a semi-invasive indolent form of infection that does not disseminate and occurs in patients who have lesser degrees of immunosuppression (such as those who take chronic glucocorticoids or those who have intrinsic immune defects) or chronic pulmonary disease. Treatment is similar to that for invasive pulmonary aspergillosis.
Aspergilloma
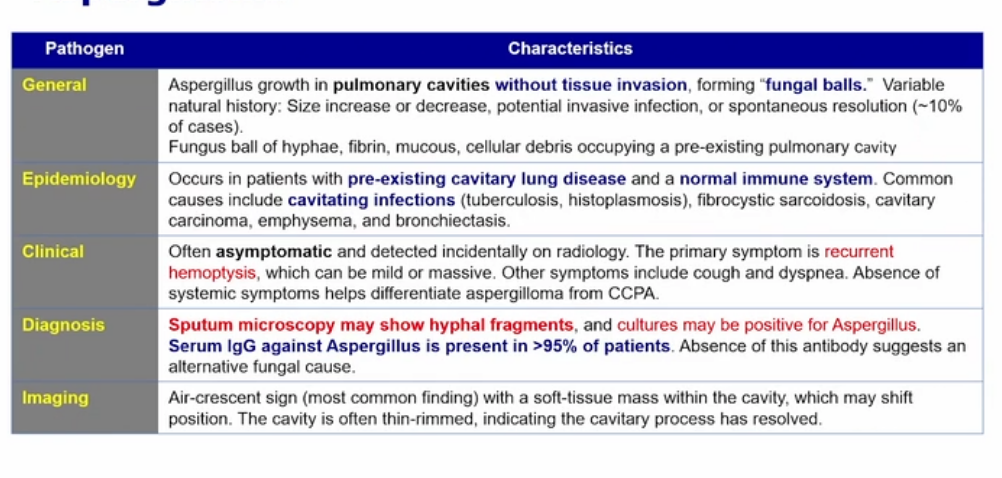
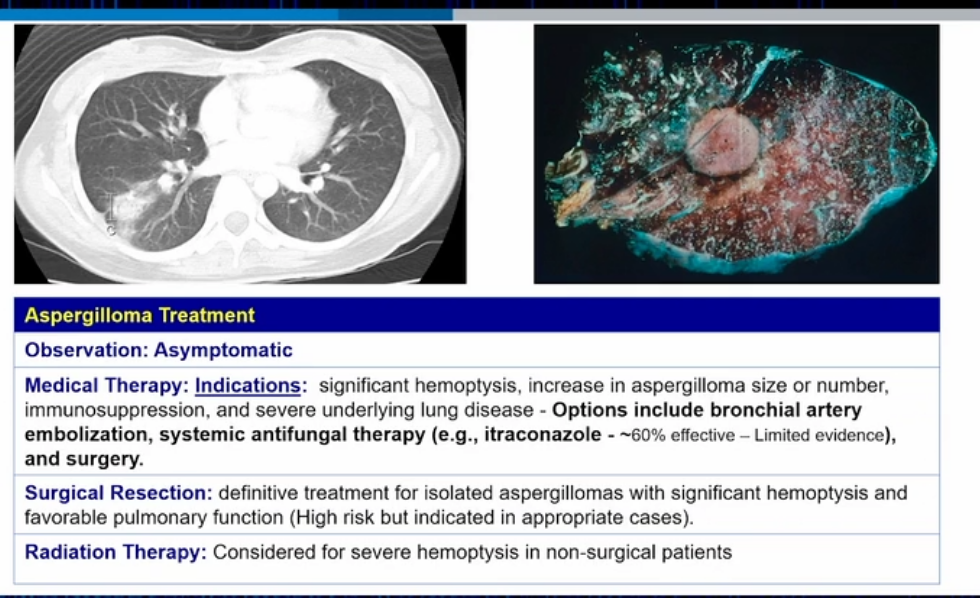
- usually not causing problem unless there’s hemoptysis with sputum showing hyphal.
- Serum IgG positive against aspergillus
- if asymptomatic do not treat
- azoles + surgery if hemoptysis Pulmonary aspergillomas (fungus balls consisting of hyphae, mucus, and cellular debris) may form in patients with pre-existing cavities, such as old tuberculosis cavities and in bullae of patients with COPD; the presence of significant hemoptysis is a potential complication. In the absence of associated symptoms or hemoptysis, pulmonary aspergillomas may not require therapy; however, in the setting of significant bleeding, surgical resection or embolization may be necessary. Antifungal therapy is typically not effective against pulmonary aspergillomas, and its role in aspergilloma treatment is unclear.
ABPA
Links to this note
-
Allergic bronchopulmonary aspergillosis ABPA
- related: Infectious Disease ID, Pulmonology, aspergillosis
-
diagnosis of ABPA includes eosinophil count, antibody level, and CT image findings
-
treat invasive aspergillosis with posaconazole
- related: aspergillosis
-
- related: aspergillosis, Infectious Disease ID