aspirin exacerbated respiratory disease
- related: Asthma reactive airway disease
- tags: #pulmonology #literature #pulmonology
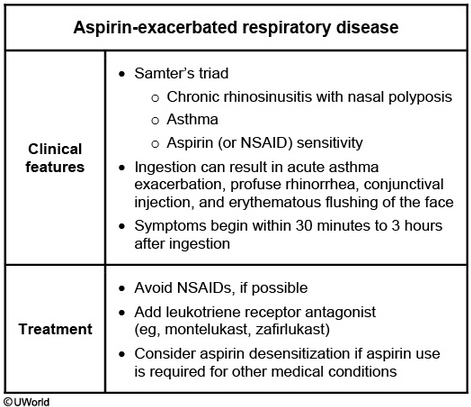
This patient’s presentation is consistent with aspirin-exacerbated respiratory disease (AERD), as summarized in the table. AERD affects up to 20% of adult asthmatics and usually presents with the classic triad of chronic rhinosinusitis with polyposis, asthma, and aspirin (or NSAID) sensitivity. Patients usually develop refractory rhinitis in their 30s followed by chronic rhinosinusitis with anosmia and nasal polyposis. The rhinosinusitis progresses to lower-airway inflammation, resulting in asthma. Aspirin and NSAID sensitivity develops during this progression. NSAIDs can induce life-threatening asthma, nasal and/or ocular symptoms, and facial flushing or erythema.
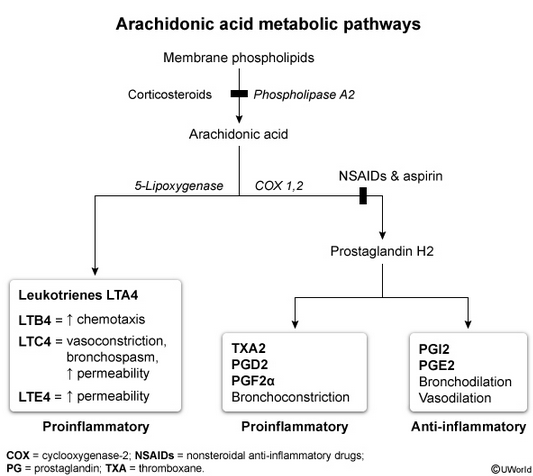
The reaction is not an IgE-mediated allergic response but is likely a shift in the arachidonic acid metabolic pathway causing excessive leukotriene production. Diagnosis is made clinically with history of aspirin or NSAID reaction. Treatment involves optimal asthma therapy, surgery for chronic rhinosinusitis, and avoidance of NSAIDs or aspirin. Current guidelines also recommend a leukotriene receptor antagonist (e.g., montelukast) to improve pulmonary and sinus symptoms. Aspirin desensitization is considered in patients refractory to therapy or who require aspirin/NSAIDs for other chronic conditions (e.g., CAD, chronic headaches).
Anti-IgE therapy is beneficial in IgE-mediated conditions such as moderate to severe asthma with perennial allergies. However, AERD is not IgE mediated.
Adding tiotropium can improve symptoms and lung function in uncontrolled asthmatics, but leukotriene antagonists are preferred in patients with AERD.1
This patient has nonsteroidal anti-inflammatory drug (NSAID)-exacerbated respiratory disease (NERD), also referred to as aspirin-exacerbated respiratory disease or Samter triad, and the gold standard to confirm the diagnosis is an oral aspirin challenge (choice C is correct). NERD is typically diagnosed clinically by a patient’s history of asthma and/or chronic rhinosinusitis with nasal polyposis, with symptoms exacerbated by NSAIDs that preferentially inhibit the cyclooxygenase 1 enzyme, including aspirin and ibuprofen. While this patient’s medical history and constellation of symptoms suggest this diagnosis, there is significant phenotypic heterogeneity of this syndrome, and presentation may vary. In addition, a study of 243 patients who thought they had NERD on the basis of symptoms reported 14% were negative for an oral aspirin challenge.
The prevalence of NERD is reported to be approximately 7% in adults with asthma and is more common among those with severe asthma. The usual clinical course starts with rhinitis, which progresses and tends to be refractory to treatment. Nasal polyposis develops and is suggested by symptoms of persistent stuffiness, difficulty breathing through the nose, and the loss of smell, as in this patient, though the diagnosis requires nasal endoscopy. Asthma that develops in adulthood usually tends to be severe. NSAID/acetylsalicylic acid (ASA) intolerance typically occurs later in the course of the disease, though may appear at any time, and symptoms generally begin 30 min to 3 h after ingestion.
The pathogenesis of NERD is believed to be related to genetic factors, with several single-nucleotide polymorphisms identified, and epigenetic factors, most notably exposure to NSAIDs. NERD is believed to result from an imbalance between proinflammatory and anti-inflammatory mediators stemming from a dysregulation of arachidonic acid metabolism, with an overproduction of cysteinyl leukotrienes and an underproduction of prostaglandin E2. Persistent type 2 eosinophilic inflammation of the upper and lower airways is a key finding, often manifested with peripheral blood eosinophilia, although this finding is nonspecific, and may be elevated in a variety of allergic disorders, infectious diseases, neoplasms, and immunologic disorders (choice A is incorrect).
Treatment of NERD centers on NSAID/ASA avoidance. Use of alternative agents such as acetaminophen or selective cyclooxygenase 2 inhibitors can be recommended to treat mild to moderate pain. Asthma management should follow standard asthma guidelines though should include leukotriene-modifying drugs because these agents have been shown to improve both pulmonary and nasal symptoms and function, with decreased need for rescue bronchodilators. Intranasal corticosteroids have been shown to be highly effective in reducing nasal inflammation and in shrinking nasal polyps, and intranasal saline irrigation, antihistamines, and decongestants may provide symptom relief. The use of biologic agents is evolving, with studies showing dupilumab being effective in improving both rhinosinusitis and asthma symptoms in patients with NERD. For those patients with conditions that require ASA/NSAID therapy, such as coronary artery disease, aspirin desensitization may be considered. Restricting alcohol ingestion is also advised based on reports that alcohol can lead to upper and lower respiratory reactions in NERD patients.
The sweat chloride test is part of the evaluation of a patient suspected to have cystic fibrosis. This diagnosis is reasonable to consider in a patient with persistent sinus symptoms suggesting nasal obstruction, though typically they are associated with recurrent infections. Furthermore, the diagnosis, while sometimes made in adults, is usually made early in life (choice B is incorrect). While asthma is a common comorbidity in cystic fibrosis patients, NSAID hypersensitivity does not generally occur.
The nasal nitric oxide test is helpful in the diagnosis of primary ciliary dyskinesia, an autosomal recessive condition characterized by abnormal ciliary motion and associated with chronic sinus infections and recurrent pneumonia, that is also typically diagnosed early in life (choice D is incorrect).2