pulmonary echinococcosis can present with pneumothorax
- related: Pulmonary Diseases
- tags: #literature #pulmonology
This patient has severe pulmonary cystic echinococcosis (CE), a zoonosis caused by the larvae of the dog tapeworm Echinococcus granulosus and therefore should be treated with albendazole (choice B is correct). In adults, cysts occur most frequently in the liver, followed by the lungs. Most symptoms of CE are caused by mass effect from the cyst volume, which exerts pressure on the surrounding tissues. The most common symptoms of pulmonary CE include cough, chest pain, dyspnea, and hemoptysis. When cysts rupture, either by spontaneous trauma or during medical intervention, protoscolices contained in the cystic fluid may disseminate into the tracheobronchial tree or the pleural cavity. Tracheobronchial involvement can lead to cough, chest pain, or hemoptysis; pleural cavity involvement can result in pneumothorax, pleural effusion, or empyema. Pulmonary CEs may also lead to a pulmonary eosinophilia, particularly in instances of rupture. This patient also had pulmonary eosinophilia as a result of tracheobronchial rupture as well as a pneumothorax and bronchopleural fistula as a result of pleural rupture of the pulmonary CE. Most often the diagnosis of pulmonary CE can be established with a combination of imaging and serology. An uncomplicated pulmonary CE appears as a well-defined homogeneous radiopacity on a chest radiograph. When it erodes into a bronchus, there is introduction of air between the pericyst and the endocyst appearing as a radiolucent rim around the cyst, as a crescent sign, on plain chest radiography and CT scanning (Figure 6). With further collapse of the endocyst, the membranes floating in the remaining fluid are known as the water lily sign (also known as the Camelot sign).
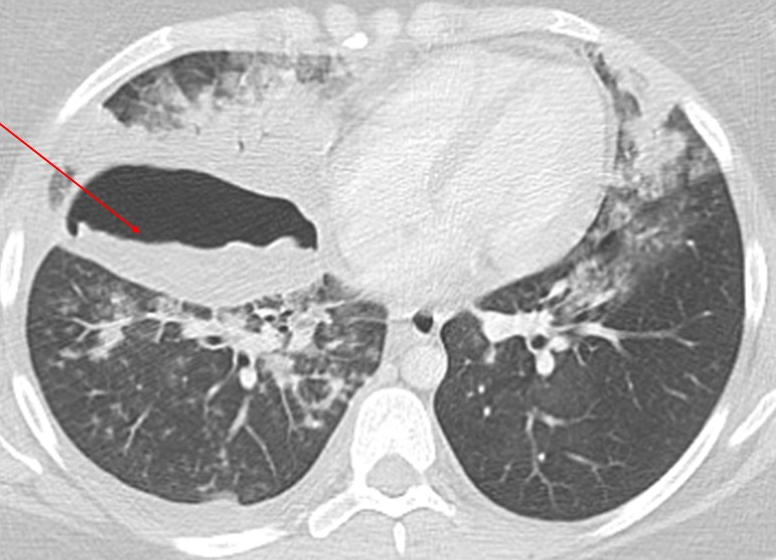
- Axial CT scan of the chest shows the ruptured pulmonary cystic echinococcosis cyst with the free-floating membranes within the cyst (water lily sign; red arrow), as well as surrounding airspace disease due to tracheobronchial rupture.
On CT imaging, intact pulmonary CEs can be difficult to differentiate from other pulmonary cysts. CT can be very helpful when there is rupture of the pulmonary CE into the tracheobronchial tree or the pleural cavity, as well as when there is secondary infection or invasion of the chest wall. Antibody detection (usually enzyme-linked immunosorbent assay) is more sensitive than antigen detection for diagnosis of E granulosus. In this case, the patient underwent surgical resection, which is the treatment of choice for complicated pulmonary CEs. The histopathology from the surgical specimen shows the host tissue encapsulating the cyst wall, which is composed of an acellular laminated layer and a nucleate germinal layer from which the brood capsule arises (Figure 7).
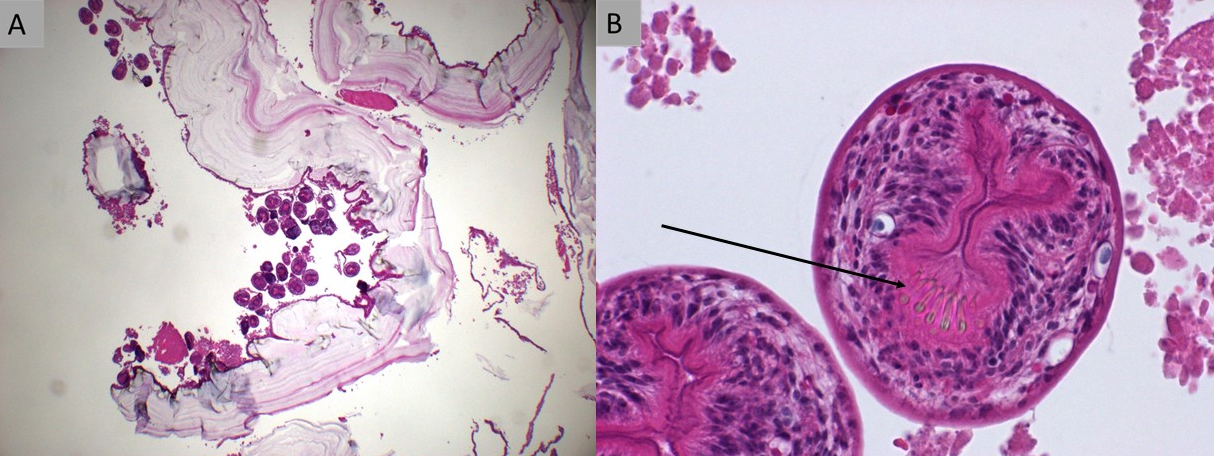
- Surgical lung biopsy specimen. A. Cross-section of the pulmonary cystic echinococcosis, stained with hematoxylin and eosin (×2 magnification), shows host tissue encapsulating the cyst wall, which is composed of an acellular laminated layer and a nucleate germinal layer from which the brood capsule arises. Inside the brood capsule are numerous protoscolices. B. Hematoxylin and eosin (×40 magnification) shows the pulmonary cystic echinococcosis protoscolex with row of hooklets (arrow).
Medical management is a useful adjunctive therapy to surgery. Albendazole is the primary antiparasitic agent used for treatment of pulmonary CE. Pyrimethamine and sulfadiazine is an effective antibiotic regimen for toxoplasmosis, which is not present in this case (choice A is incorrect). Toxoplasma pneumonia should be considered in the differential diagnosis of a respiratory illness with bilateral infiltrates on chest imaging, especially in immunocompromised hosts. Praziquantel is the treatment of choice for paragonimiasis (choice C is incorrect). Recurrent hemoptysis is the most common symptom of late infection due to paragonimiasis, with common radiologic findings including pleural effusion, hydropneumothorax, pulmonary nodules, airspace consolidation, and cysts. Ivermectin is commonly used for the treatment of strongyloidiasis (choice D is incorrect). Pulmonary manifestations of strongyloidiasis are protean and can present as pulmonary infiltrates with eosinophilia, asthma without infiltrates, hemoptysis due to alveolar hemorrhage, and hyperinfection syndrome.1
Links to this note
-
eosinophilia and lung disorders
- Parasitic infections can cause eosinophilia (pulmonary echinococcosis can present with pneumothorax, check strongyloides for peirpheral eosinophilia before starting high dose steroids).