Murray and Nadel Ch 122 Sleep Disordered Breathing Treatment
- related: Sleep and Sleep Disordered Breathing
- tags: #literature
Overview
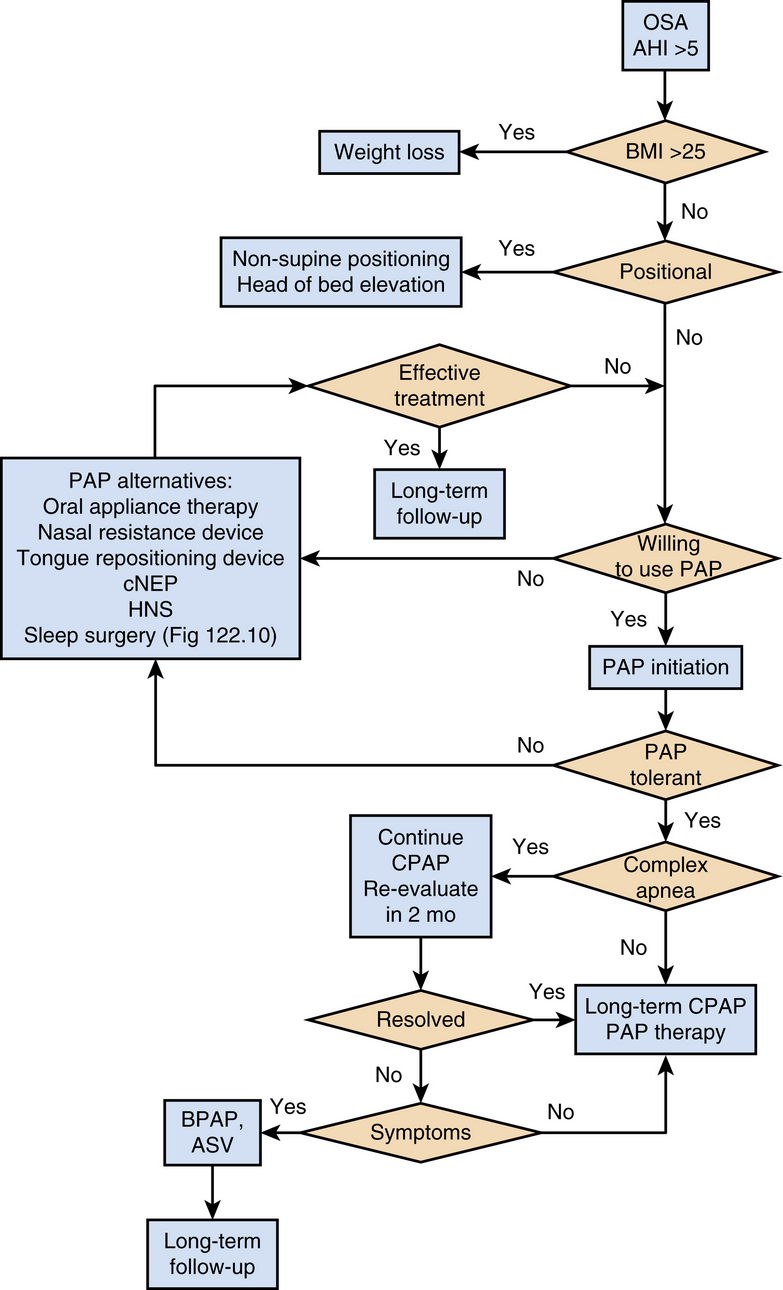
OSA Treatment
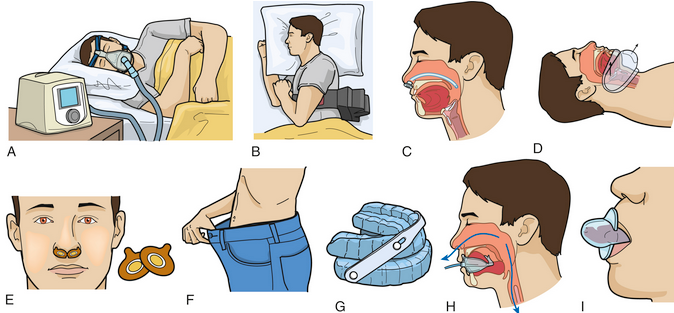
a. positive pressure b. positional device c. nasal bypass d. continuous negative external pressure therapy e. nasal resistance device f. weight loss g. mandibular advancement device h. oral pressure device i. tongue retaining device
Positive airway pressure
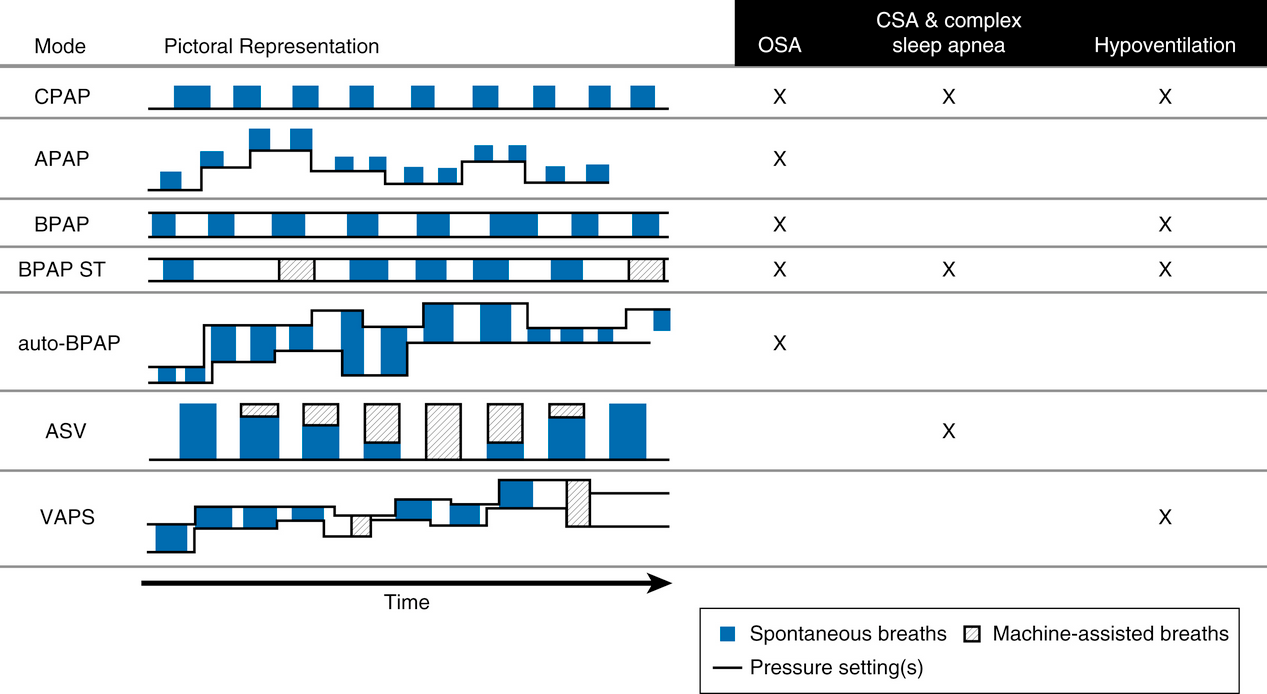
- CPAP: one pressure
- APAP: one pressure but can change throughout the night. Use for simple OSA. Don’t use for comorbidities (respiratory failure or heart failure)
- APAP can result in sleep disruption
- APAP does not work for CSA but only responds to upper airway respiratory events
- automatic PAP (APAP) and auto-bilevel PAP (auto-BPAP) senses flow, resistance and adjusts pressure automatically.
- BPAP has either spontaneous mode or spontaneous timed mode (S vs ST)
- BPAP has lower expiratory pressure compared to APAP and can be used as alternative for pressure intolerance or aerophagia
- VAPS: volume assured pressure support
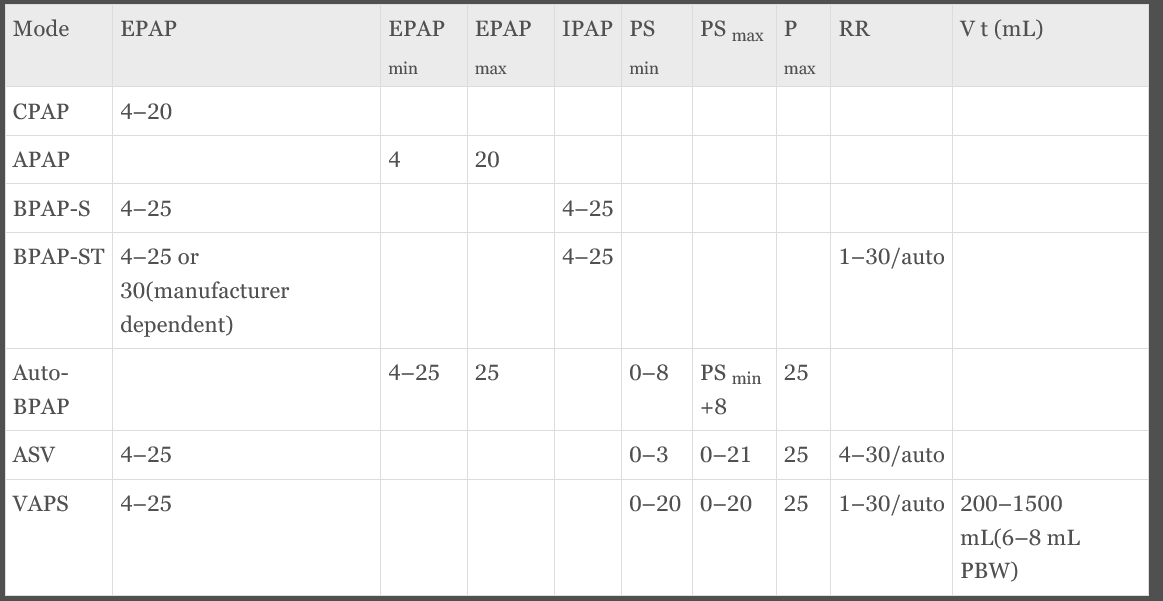
- CPAP = EPAP = PEEP; PS = IPAP − EPAP; Pmax = EPAPmax + PSmax = IPAPmax
- EPAP targets apnea. IPAP targets hypopnea
Central Sleep Apnea Treatment
CPAP
- CPAP can improve PCO2 slightly by helping VQ mismatch and reducing LV afterload
- CPAP does not improve survival benefit in heart failure patients.
Bipap
- it’s unclear whether bipap is effective
- up to 20% of OSA pts starting on CPAP can also be found to have underlying central events in the first 3 months
ASV
- adjusts each breath pressure levels
- can increase PS during apnea and hyponea; can also decrease PS during hyperventilation
Hypoventilation Treatment
- OHS, COPD, restrictive lung disease
- these require noninvasive ventilation
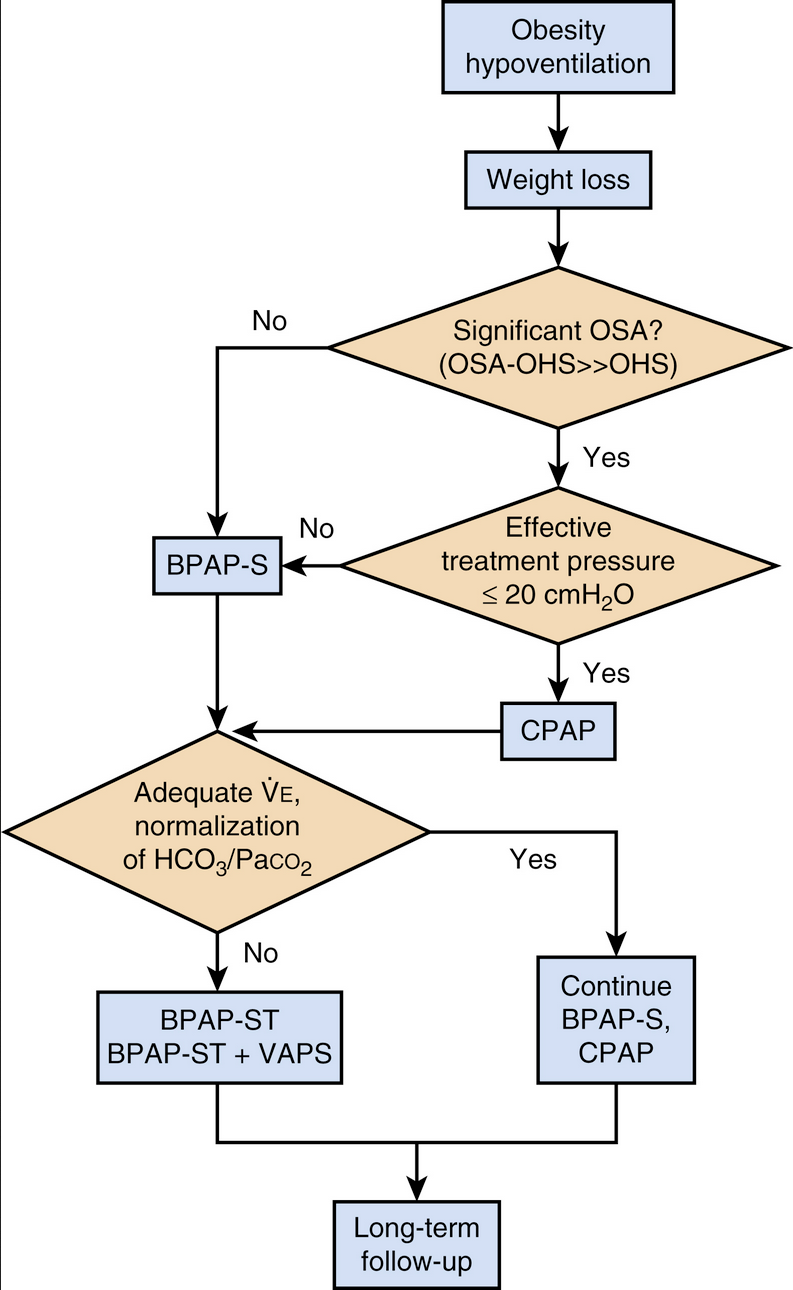
OHS
- obesity, hypercapnea, SDB
- exclude other causes for hypoventilation
- CPAP recommended initial therapy
- Bipap next
- VAPS may be tried to assure tidal volume
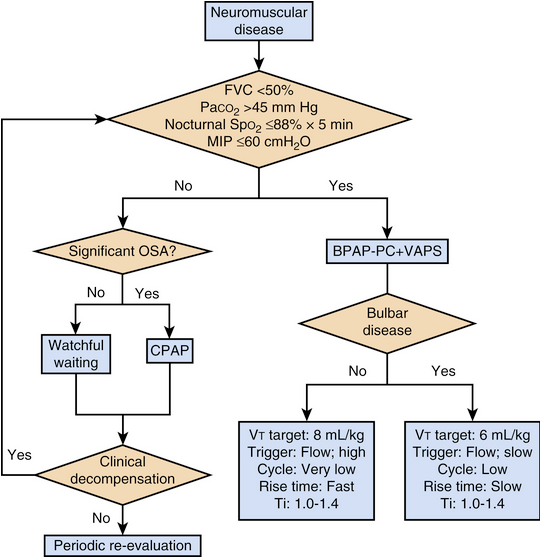
NM weakness
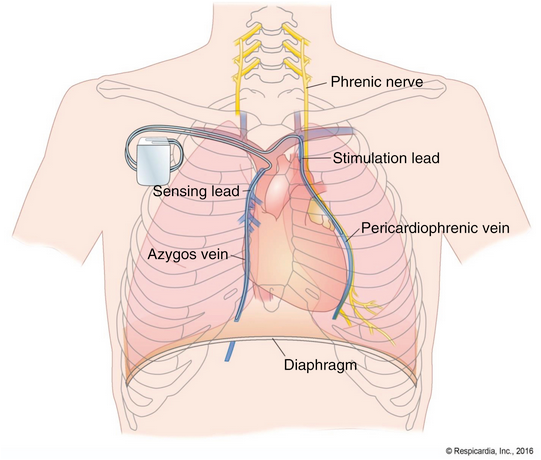
- neuro stimulator